You can help by taking a tour of the campus before school starts, encouraging your child to ask their teachers questions, and finding out who to contact at the school if issues come up. Weekly family check-ins and setting up organizing tools like color-coded folders and a homework space at home can also make a big difference.
The post From Roundtables to Global Panels: Youth Mental Health Commands World Stage for International Youth Day 2025 appeared first on Child Mind Institute.
]]>New York, USA and Brasília, Brazil — The Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute is mobilizing young advocates and cross-sector stakeholders for International Youth Day 2025. In celebration of this day, two high-impact forums designed to strengthen youth mental health care policy and systems will take place.
Under the theme Youth Advancing Multilateral Cooperation Through Technology and Partnerships, children and adolescents are not only joining conversations about mental health care, but also leading them. On August 9, the SNF Global Center is partnering with youth advocates, policymakers, diplomats, and innovators during the 30th annual AFS Youth Assembly panel, “Beyond the Surface: The Global Mental Health Crisis” in New York. The discussion will explore global youth mental health, with a particular spotlight on the impact of pandemics, armed conflicts, and climate change.
The flagship conference of the AFS Intercultural Programs will be held on August 8-10 and is expected to attract approximately 700 young leaders (ages 18-35) from over 100 countries. This includes those working in grassroots as well as international development towards sustainable transformation. The AFS Youth Assembly, a non-profit organization promoting global citizenship, youth engagement, and collaborative impact, has been supporting young leadership for more than 100 years.
“We are proud to take a leading role in this critical conversation to advance the improvement of culturally responsive and evidence-based solutions in resource-limited settings. Through the right platforms and support, young people continue to powerfully demonstrate that the future of mental health care is through inclusivity, technology-driven solutions, and international collaborations,” said Eduardo Vasconcelos, Youth Engagement director at the SNF Global Center.
On August 12, Vasconcelos will also co-lead two panel discussions in Brazil, focused on youth leadership, mental health, and public policy as part of an official congressional celebration. The event in Brasília will convene youth advocates, parliamentarians, government officials, and civil society organizations to exchange ideas, highlight best practices, and promote inclusive and science-based policymaking. This year’s call to action is to recognize mental health as a central pillar of youth development and a necessary focus of Brazil’s National Youth Policy.
This collaborative initiative is organized by the Brazilian Congressional Caucus on the Promotion of Mental Health, the Secretary for Infancy, Adolescence, and Youth of the Chamber of Deputies, and the Institute for Health Policy Studies (IEPS), in partnership with the SNF Global Center. The idea for the event was first proposed by the nonprofit Young Peacebuilders, an organization partnering with the SNF Global Center that works to prevent school-based violence and promote mental well-being among Brazilian youth.
The SNF Global Center has mobilized members of its Youth Council in Brazil, including Ana Beatriz Araujo, Júlio Ruan, and Daniel Nascimento, who will join as speakers and participants in the panels, while also engaging directly with legislators and sharing critical insights from their experiences at the local and national levels.
The first roundtable, “The National Youth Policy in Dialogue with Parliament,” will open the event to examine Brazil’s current youth legislation and the intersection of mental health, inclusion, and environmental sustainability. The final session titled, “Youth Mental Health in Perspective,”will feature youth advocates, health professionals, and grassroots leaders to discuss Brazil’s most pressing mental health challenges.
The event will also mark the launch of two major papers published in the Stanford Social Innovation Review Brasíl, both addressing the state of mental health for children and adolescents in school communities. One is produced by the IEPS and the second is co-authored by experts from the SNF Global Center, offering evidence-based insights into how children and adolescents’ mental health can be better supported in schools.
“What makes the events in Brazil and New York unique is the anticipated creation of concrete pathways from lived experience to system change through youth expertise, ensuring policies reflect actual needs,” said Joseph Elias, managing director, SNF Global Center. “We are also looking forward to previewing findings from two studies aimed at filling critical knowledge gaps and challenging how global youth mental health is understood.”
Mental health is a fundamental aspect of well-being, yet it remains one of the most overlooked global health challenges, especially in low and middle-income countries where 90 percent of the world’s children live. Both International Youth Day events provide an opportunity for generational bridge-building and a platform for youth to lead.
About the SNF Global Center at the Child Mind Institute
The SNF Global Center brings together the Child Mind Institute’s expertise as a leading independent nonprofit in children’s mental health and the Stavros Niarchos Foundation (SNF)’s deep commitment to supporting collaborative projects to improve access to quality health care worldwide. The center is building partnerships to drive advances in under-researched areas of children and adolescents’ mental health, and expand access to culturally appropriate training, resources, and treatment in low- and middle-income countries. This work is conducted by the Child Mind Institute with support from SNF through its Global Health Initiative (GHI).
About the Child Mind Institute
The Child Mind Institute is dedicated to transforming the lives of children and families struggling with mental health and learning disorders by giving them the help they need. We’ve become the leading independent nonprofit in children’s mental health by providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing tomorrow’s breakthrough treatments.
The post From Roundtables to Global Panels: Youth Mental Health Commands World Stage for International Youth Day 2025 appeared first on Child Mind Institute.
]]>The post Selective Mutism and Starting Kindergarten appeared first on Child Mind Institute.
]]>Some kids with SM may have made progress talking in preschool, but will still find it challenging speaking to a brand-new kindergarten teacher, for example. And finding their way around a new building and classroom can be particularly hard if they aren’t able to speak up to ask for help. Fortunately, there are steps that parents can take to help children with SM have a more successful transition into kindergarten.
Communicate early with the school
Most schools won’t send out a child’s kindergarten teacher assignment or the class list until close to the start of the school year. If you have a child with SM, you’ll want to reach out to school staff earlier. If you don’t know your child’s teacher assignment yet, you can reach out to the principal and school psychologist/counselor to do the following:
- Share information about SM. If you have a child with a diagnosis of SM, it is important to share this information with your child’s new school. Transparency is key to foster empathy, understanding, and a team approach. Not all educators are familiar with SM, so it can be helpful to share information about what SM is, in addition to some of the “dos and don’ts” for supporting a child with SM at school. Our Teacher’s Guide to Selective Mutism is a great place to start!
- Give a fuller picture. You want the staff at the school to know your child, not just their SM struggles. Sharing information about your child’s interests and a video of your child talking and playing normally at home can help the school get a full picture of your child, beyond the SM.
- Connect your team. If your family is working with an outside therapist or counselor, you’ll want to introduce them to your child’s new school as well. They may be able to provide additional training or resources for school-based staff.
- Ask about supports. It’s a good idea to ask the school if they’ve had other students with SM before, and what they may recommend or require of you to provide the supports your child needs. States and school districts have different ways of evaluating and intervening when an anxiety disorder impacts a child at school. Some schools may recommend a Section 504 plan or Individualized Education Program (IEP). Parents interested in formalizing accommodations or interventions for their child with SM can ask schools for more information and request a 504 plan or IEP evaluation, if applicable.
Build comfort before school starts
Children with SM fare best when we take steps to help them build familiarity with new people and places in a gradual way. Reach out to your child’s school and let them know that your child will be much more comfortable if they can meet the teacher briefly and see the classroom before the crowded, chaotic first day. Some schools even offer orientations or “meet the teacher” days for all incoming kindergarteners!
- Arrange a school and classroom visit. Bringing your child for a visit to school ahead of the first day gives them the chance to get comfortable there, especially if they can check out their new classroom and other important places (e.g., the bathroom, their cubby, where they’ll be dropped off). When you have a child with SM, you’ll want to see if you can get your child talking to you in the school building and in their new classroom. Having successful experiences talking to you in the classroom can help pave the way for “brave talking” progress at school.
- Meet with the kindergarten teacher. Try to find a brief time when you and your child can meet the new teacher. Not all children will be able to talk to the teacher during this first interaction, and that is okay. Maybe you bring your child’s favorite game along and play together, which takes some of the pressure off and provides structure, predictability, and a sense of familiarity for your child. If your child is able to talk to you in the presence of the teacher and seems ready for it, maybe you give the teacher a question to ask your child. You can have your child answer those questions at home beforehand to build confidence through practice.
- Connect with classmates. You may know some kids from the neighborhood or from your child’s preschool class who will be starting kindergarten at the same school. If you’re able, setting up playdates or coordinating times to meet up at the park together is a great way to help ease your child’s transition into kindergarten. If your child is ready, try to build their comfort and get them to talk in front of or directly to their classmates. No matter what level of talking happens, your child will benefit from the extra familiar faces on day one!
Plan ahead for appropriate accommodations
Appropriate accommodations for a child with SM are temporary supports that reflect what a child needs to set them up for success at school. This might include things like using alternative forms of communication (e.g., the use of nonverbal signals or communication cards) or regular prompting for bathroom breaks, among others.
As kids make progress speaking at school, we want to gradually reduce these accommodations. This helps your child become more confident in the classroom and continue making progress toward overcoming SM. For example, a child who can speak to their teacher and classmates should not be using communication cards in the classroom, but they may still need the cards to communicate with their teachers in special classes like art and music. The appropriate level of accommodations can be challenging for parents and schools to determine — mental health professionals with expertise in SM can give guidance.
Every child is going to be in a slightly different place on their SM journey at the start of kindergarten. Though some back-to-school stress may still be inevitable, communicating with the school and planning ahead to ensure your child has the supports they need can ease your child’s (and possibly your own!) anxiety.
The post Selective Mutism and Starting Kindergarten appeared first on Child Mind Institute.
]]>The post Raising Good Humans: Cognitive Behavioral Therapy At Home get home (CBT): Practical Tools for Families with Dr. David Anderson appeared first on Child Mind Institute.
]]>The post TODAY: Why Do Kids Totally Lose It After School? All About Restraint Collapse appeared first on Child Mind Institute.
]]>The post Family-Focused Therapies for Bipolar Disorder appeared first on Child Mind Institute.
]]>What bipolar disorder looks like in kids and teens
Bipolar disorder in young people doesn’t always look the way you might expect. In adults, it’s often described as alternating episodes of mania and depression. In kids, things can be more rapid, more chaotic, and harder to pin down, explains Mary Fristad, PhD, an expert in mood disorders in children at Nationwide Children’s Hospital and professor emerita at The Ohio State University.
“A real red flag,” says Dr. Fristad, “is when kids, for several days on end, have increased energy — what I call ‘the too much.’ They don’t need to sleep as much. They have too much energy. They’re intrusive, in your face, their speech is louder and faster, and they’re not backing down in a way that doesn’t fit the situation.” She explains that this kind of behavior goes beyond typical childhood excitement. A kid staying up late because they’re excited about a birthday? That’s normal. But a kid who’s up at 2am reorganizing their bedroom or calling every number in their parent’s contact list — and isn’t tired the next day? That is likely something more.”
Dr. Fristad has also seen kids who unlock the door and wander the neighborhood in the middle of the night, or eat all the cheese in the refrigerator. “These are all examples I’ve seen,” she says. “And they can be very concerning if you don’t know what you’re looking at.”
Most diagnoses in young people happen in adolescence, after puberty, but Dr. Fristad has worked with kids as young as eight (and occasionally even younger).
Why catching it early matters
Ideally, kids with bipolar disorder can be identified before they have an full-blown episode of mania or depression. It’s possible to catch it during what experts call the “prodrome,” a period when early warning signs appear. “In the prodromal phase, we might see mood swings, irritability, sleep disruption, or anxiety,” Dr. Fristad explains, “but those symptoms are nonspecific — they could lead to bipolar disorder, or they might not.” That’s why careful monitoring and early intervention are so important, she adds: “The goal is to catch kids who are at high risk and provide support before symptoms get worse or more entrenched.”
Getting help early doesn’t necessarily prevent the condition, which runs in families, from developing. But it can delay more serious episodes and give kids time to develop healthy coping skills. “If it doesn’t show up until they’re 25 or 30 instead of 10 or 15,” she says, “think about how different that person’s life will be. They finish school. They build a healthier sense of self. They’ve developed ways of interacting with authority figures that work. That is a gift.”
Therapies for bipolar disorder
For young people with serious symptoms, therapy is usually recommended along with medication. There are three well-established forms of a type of therapy called Family Psychoeducation Plus Skill Building, which engages parents and other family members to help kids and teens with bipolar disorder:
- Family-Focused Therapy (FFT)
- Child- and Family-Focused Cognitive Behavioral Therapy (CFF-CBT)
- Multi-Family and Individual-Family Psychoeducational Psychotherapy (MF-PEP, IF-PEP)
Each one has a slightly different structure, but they all share a core approach: teaching families about the disorder and building skills together. “You can quibble over the differences,” Dr. Fristad says, “but they’re really cosmetic. It’s much more impressive that we’re all doing the same thing. These therapies are not just about understanding the diagnosis, they’re about giving families something they can use every day.”
What kids and families learn
All of these examples of Family Psychoeducation Plus Skill Building focus on a few key things:
Understanding mood symptoms
Families learn how symptoms show up in kids and how to recognize when things are starting to shift. “Kids and parents need to understand the symptoms and have a common language to talk about them,” says Dr. Fristad. “They need to be able to talk about it in a matter-of-fact way.”
Better communication
Parents and kids practice ways to talk that reduce conflict and improve understanding. “We want kids and parents to move from blaming to problem-solving,” says Dr. Fristad. That might mean using “I” statements (for example, saying “I feel…” or “it feels to me like…” rather than blaming the other person) or learning how to pause and take a break during a heated moment.
Emotion regulation tools
Kids learn coping strategies to calm down when they feel themselves getting stressed or upset. Dr. Fristad likes the acronym CARS: Creative, Active, Relaxation, and Social. These might be drawing, playing music, going for a walk, or texting a friend. The goal is to help kids recognize when they’re getting dysregulated and have options to help themselves get back on track. “We also spend time helping kids figure out what works for them specifically,” she says. “Some kids calm down with music. Some need to run around. Some just need to be left alone. We help families figure that out together.”
Problem-solving and planning
Families work together to make a plan: What are the early signs that a mood shift is coming? What should we do when that happens? “If you’re keeping a mood and medication log, you might find that flare-ups always happen when there’s a particular school stressor,” says Dr. Fristad. “That tells us we don’t need more medication — we need to address the problem at school.” Planning might also mean keeping track of sleep and sticking to a routine, while also being open to flexibility as situations arise. Again, the awareness of symptoms helps families plan to manage them.
Group vs. individual therapy
Family-focused approaches can happen one-on-one or in a group setting. Both can work well, but groups add something extra — connection. “Parents get so much support from seeing other parents who are in the same difficult situation,” says Dr. Fristad. “You look around the room and think, ‘Oh, you’re not a bad parent — and yet your kid gets out of control just like mine.’”
Kids benefit from that connection, too. “When kids hear another kid say, ‘I don’t sleep when I’m hyped up’ or ‘I cried all day for no reason,’ they realize they’re not alone.”
One activity Dr. Fristad uses with kids involves writing their strengths in one column on a piece of a paper and their symptoms in another. Then they fold the paper so only the strengths are visible. “The point of treatment,” she says, “is to put the symptoms behind you so the real you shows up.” And group settings help with stigma, too. “Families often feel so isolated. Being around others who get it — who truly understand — that’s powerful.”
If group therapy doesn’t work for a family, because of scheduling or privacy concerns, the same material can be covered in individual family sessions. “We meet families where they are,” says Dr. Fristad. “The important part is that they get the information and support.”
Where medication fits in
For most kids with bipolar disorder, therapy is combined with medication, which can include traditional mood stabilizers, such as lithium or valproate, and/or atypical antipsychotic medications. Part of therapy is helping families keep track of how things are going and communicate clearly with their prescriber. “We don’t prescribe medication in these therapy sessions,” says Dr. Fristad, “but we help families become better consumers of care.” That might mean keeping a log of side effects or noting when symptoms change.
Some kids with mild symptoms might be able to manage with therapy alone — especially if they have strong routines around sleep and nutrition. She emphasizes sleep as a treatment target: “We spend a lot of time helping families improve sleep hygiene because poor sleep can tip a kid into an episode. Sometimes fixing that piece makes a big difference.”
Other treatment options
In addition to the core therapies she’s developed and studied, Dr. Fristad notes there are other promising approaches that may help some children with bipolar disorder.
One is dialectical behavior therapy (DBT), originally developed for adults with borderline personality disorder. “DBT has a lot in common with what we do in family-focused therapy,” says Dr. Fristad. “It’s skills-based, it emphasizes emotion regulation, and it brings the family into treatment. It just uses a slightly different framework.”
Another is interpersonal and social rhythm therapy (IPSRT), a treatment that focuses on stabilizing daily routines like sleep, eating, and social activity to help regulate mood. It also addresses interpersonal stress by improving relationships and coping with life changes. By combining routine regulation with therapy for relationship challenges, IPSRT helps reduce the risk of future mood episodes. Family Psychoeducation Plus Skill Building also incorporates core principles of IPSRT, including regulating sleep and improving family relationships to reduce stress.
The takeaway for families
Therapy doesn’t fix everything overnight. But it can give families a sense of direction — and help kids feel more understood and in control. “You didn’t cause it,” Dr. Fristad tells parents. “But you can improve the course of it.” And to the kids, she says, “It’s not your fault, but it is your challenge. If you don’t learn the strategies to manage these symptoms, they have the potential to really mess up your life. And we don’t want that to happen.”
The post Family-Focused Therapies for Bipolar Disorder appeared first on Child Mind Institute.
]]>The post Parade: Child Psychologists Say These 9 Phrases Are Doing More Harm Than Good—Even if You Mean Well appeared first on Child Mind Institute.
]]>The post Parade: Child Psychologists Say These 9 Phrases Are Doing More Harm Than Good—Even if You Mean Well appeared first on Child Mind Institute.
]]>The post PopSugar: The Summer’s Hottest Parenting Hack? Boredom appeared first on Child Mind Institute.
]]>The post PopSugar: The Summer’s Hottest Parenting Hack? Boredom appeared first on Child Mind Institute.
]]>The post Starting Middle School appeared first on Child Mind Institute.
]]>Clutching my freshly printed class schedule as a lifeline, I rushed through the double doors to find my locker (no more cubbies for me!) and my friends. I was immediately hit with the smell. An intense mixture of body odor, Axe body spray, Juicy Couture Viva La Juicy perfume, and ammonia.
And pressed up against the lockers — adjacent to my newly assigned one, unfortunately — was a couple aggressively making out. The boy had his hand fully up the girl’s shirt and showed no signs of stopping, despite the deluge of kids rushing to get to first period before the bell. Clearly, middle school was going to be a very different experience.
What are the big changes?
The transition from elementary school to middle school can be both exciting and challenging for kids. They’re entering a new school structure that pushes them to take on more responsibility and a heavier workload. And as they start puberty, they’re going through physical, hormonal, and emotional changes that impact their sense of self as well as how they interact with their friends, classmates, and family.
“I work with a lot of fourth and fifth graders and, towards the end of the year, we have a lot of conversations about anxiety around going to middle school,” says Emma Petree, LMSW, a social worker for School and Communities Programs at the Child Mind Institute. “The things that I hear the most are worries about switching classes, an increase in workload and homework, and more exposure to substances, like smoking and vaping.”
A change in class structure
Among the most jarring parts of transitioning to middle school is the change in class structure. Instead of having one teacher throughout the day, kids have multiple teachers for different subjects. Keeping track of their class schedule, traveling between classrooms in a short amount of time, and storing their things in a locker can be a lot to handle (I lost my locker’s padlock a few times, I’ll admit).
It can be helpful for students to have exposure to the physical campus before they get there, says Ms. Petree. “A lot of schools do back-to-school days before they start school. I think that is so helpful to alleviate anxiety.”
You can explain to your child that since they’ll have a different teacher for each subject, classes may have varying levels of difficulty in terms of assignments, grading criteria, and expectations. Encouraging them to go to their teachers (or a school advisor, if they have one) when they have questions or specific issues with assignments can help them feel more independent.
Though you can still be prepared to step in, working with their teachers or other school staff to figure out your child’s specific needs and offer the right support.
“This is a big transition for parents too, because in elementary school you have one go-to teacher you can e-mail about any questions or problems,” says Janine Domingues, PhD, a senior psychologist in the Anxiety Disorders Center at the Child Mind Institute. “You’ll have to find out who you can reach out to, whether it’s an advisor, a school-based counselor, or specific teachers.”
How do you help your child stay organized?
In middle school, kids experience an increase in homework assignments, tests, quizzes, and projects. They’ll also need to manage their time. “Middle school is the first time where kids need a lot more executive functioning skills,” says Jane Wong, PsyD, an associate neuropsychologist in the Gund Learning and Diagnostic Center at the Child Mind Institute.
Dr. Wong recommends getting different colored folders for each subject, as well as a calendar for assignments, to help kids visualize when things are due. And she suggests making a checklist to help kids figure out what they need to put in their backpack each morning.
Established routines for homework, including a dedicated workspace at home, are essential. And for kids with ADHD or attention issues, says Dr. Wong, you can get a Bouncyband for their chair or a wiggle seat, to help them focus.
Dr. Domingues notes that it’s important to give kids some grace, since this increase in responsibilities can be overwhelming. “I recommend that parents, especially early on, set a time each week where you’re touching base with your kid,” she says. “You can ask questions like, ‘How did this week go?’ ‘Were there moments where things felt really chaotic? So that way, you can check in without feeling like you’re hounding your kid every day.”
Shifts in friendship dynamics
Starting middle school often leads to a shift in friendship dynamics, whether this means making new friends or drifting away from old ones.
“This is a time for friendship exploration, and it comes with some pain,” says Dr. Domingues. “It’s a time where you’re exploring who you are and what you want out of friendships. That’s all very normal.”
For some kids, these changes can bring on a lot of anxiety, Dr. Domingues explains, while others embrace the chance to explore.
With kids who are actively seeking new friendships, says Dr. Domingues, it can be helpful for parents to have conversations around who they might be gravitating towards and what they’re looking for in a friend. “And if they’re branching out you also want to make sure they’re still being kind. Talk to them about how they can have a healthy separation from a friend, as opposed to ghosting or just pulling away without a discussion.”
And if you notice that your kid is reluctant to make new friends, Dr. Domingues says that you can validate their feelings, discuss what they’re worried about, and reassure them that meeting new people often feels awkward at first. “Go over ways they can branch out, whether it’s joining different groups or clubs at school, sitting at a different table at lunch, or joining an activity outside of school.” She also mentions coaching kids on how to open a conversation, like asking someone about their weekend plans or talking about a class or a teacher you have in common.
“And I often say, you don’t have to be friends with everyone,” says Dr. Domingues. “It just takes one person you really connect with.”
Peer pressure
As kids are forming these new connections and friend groups, they might start to feel as if they need to act or look a certain way to fit in.
“This is when peer pressure gets really intense,” says Ms. Petree. A child’s social circle, she says, tends to move to the “forefront of their decision-making.”
Both Ms. Petree and Dr. Domingues agree that establishing family values can help kids handle situations in which they might be pushed to do something they aren’t comfortable with.
“Something that lands with this age group is values-based conversations and really emphasizing kids’ sense of self,” says Ms. Petree. “They’re at the very beginning of starting to form their identities, and they’re still really young. Maintain a set of values to live by where it’s not just, ‘Don’t do this,’ because they’re not hearing that. This way, they can make decisions for themselves, and feel a sense of independence and autonomy, which is what they’re also really craving.”
“I think it’s also about language and scripting sometimes, too,” Dr. Domingues adds. “Kids don’t always know what to say, when to say no, or how to say no while still maintaining a friendship. So, parents can practice these types of conversations with their kids.”
Body image insecurities
When kids enter middle school, they’re usually starting or already going through puberty. And with puberty comes a host of bodily changes that can lead to anxiety and insecurity.
It was in middle school gym class that I first became acutely aware of my body and its shortcomings. We’d have to change in front of each other in the locker room and girls took the opportunity to compare and comment on each other’s “progress.” Discussions about bra sizes, hip width, and shaving were common.
Many states still require kids to take physical fitness tests, which can involve public weigh-ins and BMI reporting.
To prepare kids for these types of uncomfortable scenarios, parents can initiate conversations about puberty and bodily changes early, says Dr. Domingues. “Talk to your kid about how everyone’s body is different, and make sure they understand what puberty actually means — what your body looks like right now isn’t how your body’s going to look like two or three years from now. This validates their experience.”
Having broader conversations around beauty standards and ideal body types with your child, she adds, can also really make a difference in how your child navigates this new environment.
Exposure to sexual pressure
Kids starting middle school are more likely to be exposed to sexual content and substance use, Ms. Petree warns. “I think just by virtue of being around older kids, they’re exposed to a lot more really quickly. Social media and internet access definitely plays a huge role in that.”
Dr. Domingues encourages parents to have conversations about these topics early, even in fourth or fifth grade, before they start middle school.
Because along with exposure can come pressure. “With young girls, especially, I often see that the combination of this new exposure — along with peer pressure and hormonally influenced self-esteem struggles — means that they’re getting in situations that are potentially risky or harmful,” Ms. Petree observes.
She describes working with a lot of girls who think that they owe sexual behaviors to other people. “We have a lot of conversations about empowerment and repeating phrases such as, ‘You don’t owe anyone anything. Your body is yours and your choice.’”
Ms. Petree also frequently advises young girls to “tune in” to their bodies and notice when things are comfortable versus uncomfortable. “Again, saying, ‘Don’t do this,’ isn’t going to work,” she explains. “Instead, really teach kids to listen to what feels safe and not safe in their bodies.”
Conversations about space and boundaries can be just as important for boys, says Dr. Domingues. “I think that boys can be physical with one another too. And it might not even be sexual. It could be like roughhousing or rough play. Some kind of crossing of boundaries that can make people uncomfortable.”
Boys can also feel pressured into sexual activity that they may not be comfortable with because they’re seeing their peers doing it, she adds.
Parents can talk to their kids about how to speak up if they see problem behavior, and help them get comfortable sticking to what feels respectful.
Frequently Asked Questions
Many kids worry about switching classes, managing a heavier workload, and dealing with lockers. They’re also going through puberty, which brings physical, emotional, and social changes. Friendship dynamics shift, peer pressure increases, and they may be exposed to new situations involving sex or substance use.
Take advantage of back-to-school days to walk the campus. Help your child stay organized with folders, checklists, and a calendar for assignments. Set a weekly time to check in with them. Encourage honest conversations about boundaries, body changes, and how to navigate new friendships.
Give them some grace. This is a big change. Set up a weekly time to talk about what’s going well and what’s feeling overwhelming. If they’re struggling socially, talk through ways they can branch out—like joining a club or asking someone about a shared class. For academic concerns, work with teachers or school staff to support them.
The post Starting Middle School appeared first on Child Mind Institute.
]]>The post Starting High School appeared first on Child Mind Institute.
]]>“I think it makes sense to think of freshman year as distinct from the other three,” says Jenna Klorfein, LCSW, who was a social worker in a New York City high school. “There’s a general kind of fish-out-of-water feeling, like, ‘I’m trying to make sense of all of this.’” It can take time for a teen to find their place, both academically and socially, but parents can help by preparing for some of the more common challenges of freshman year.
Mastering new routines
In the first days and weeks of school, some of the biggest stressors will be logistical. For example, most freshmen will be encountering a new building, often much larger than the one they were used to — and learning to confidently navigate unfamiliar hallways through a sea of bodies can take some time.
Another daily challenge is the commute. If your teen is using public transportation to get to school, help them practice the route they will take to get there, especially if they’re regularly traveling by themselves for the first time. And if the high school is farther from home, consider whether that means earlier wake-up times than they’re used to. If they take medication for ADHD, they’ll need to figure out what time is best for them to take it.
Getting used to a new entry protocol can be a struggle, too. The high school where Klorfein worked is housed in a building with multiple other schools, and kids have to go through a metal detector to get in. So, if your teen tends to get overwhelmed by noise or crowds, for example, make sure they understand that certain elements of their school day — which will already be unfamiliar — might feel uncomfortable at first, too.
Handling more responsibility
In high school, teens will mostly be expected to keep up with deadlines and assignments on their own. “If you don’t get your work done, nobody’s going to say, ‘Hey, you have to turn that in.’” Klorfein says. The idea is to teach freshmen to be responsible for their own work — which can be especially tough for teens with ADHD, learning disabilities, or executive function issues.
One challenge for freshmen is getting used to studying for tests or researching and writing a paper over time. Wendy, whose son Ralph is a high school junior in Ohio, says this was a particularly difficult transition. “He’d say it will take an hour when it actually takes three days,” she jokes (sort of).
But as Wendy also points out, teens need help learning what they don’t know — teaching them how to set aside time for studying over multiple days, for example, so later they can do it on their own.
“In high school, the parent becomes like an adviser,” Wendy says. “The goal is for them to become obsolete, but it takes a huge amount of work to get there.”
New academic pressures
Whether your teen breezed through middle school or they struggled, they should expect classes in high school to get more challenging. Students will do more reading in every subject. They will also learn more complex math concepts that build off of one another — which can be difficult to absorb and recall on a semester schedule. (How am I supposed to remember how to do algebra? I haven’t heard the word “variable” in a year.) And of course, a student’s grades will officially “count” toward graduation.
Some kids may need to be reminded of this — and also that the extracurriculars they love, including sports and things like marching band and theater, often require a minimum GPA for participation. Poor grades early take more work to recover from later on, so make sure your teen has whatever learning support they need as early as possible so they can pursue the things they truly enjoy.
But those incoming freshmen who are already worried about their college application may be painfully aware of the new importance of grades. Help them set realistic expectations and a healthy mindset, early. Try to focus your praise on their efforts and personal achievements. Maybe they got much more confident speaking French or learned a cool photo editing technique. While you can’t make overachievers forget they got a B on a test one time, you can help them see that a good grade isn’t the most important thing.
If your child struggled to make friends in middle school or was bullied, they might be anxious about the high school social scene. When talking to them about it, Klorfein suggests “reframing it as an opportunity to find more people like you.”
Maybe your teen is already a star athlete and shoo-in for the volleyball team. But for teens with less committed interests, encourage them to choose a club or team and join it. If they’re resistant, ask them to pick one extracurricular and try it for a certain amount of time. They do not have to be an Olympic swimmer or obsessed with photography — the point is for them to expand their social circle. If they find something they’re truly passionate about or uncover a hidden talent, that’s a bonus.
Ralph joined the soccer team his freshman year, and Wendy says it has been an important part of his social experience. “It means he has multiple groups of friends,” she says. Teens will inevitably experience friendship volatility in high school; it’s easier to endure when you have different people to call on.
That said, it can take time for freshmen to settle in socially — and that’s totally normal, Klorfein says. “How you spend freshman year is not how high school is going to be” just given the size of the adjustment, she says. “So, if it’s hard for you, or you haven’t found your people by the end of the year, that’s okay.”
Encountering adult stuff
While most 14- and 15-year-olds are not completely naïve about sex or drugs, mixing with older teenagers (while a good thing) can put them in contact with more adult stuff than they encountered in middle school. “There’s a different level to it in high school,” says Katie Peinovich, LCSW, a licensed clinical social worker at the Child Mind Institute. “Drugs are in every school — it doesn’t matter where it is. They all have kids vaping in the bathroom.”
A lot of times parents don’t want to talk about drugs or other uncomfortable topics and will wait to deal with issues as they come up, Klorfein says. But both Peinovich and Klorfein stress the importance of having proactive conversations with your teen about sex and drugs, which means giving them the information and tools to handle situations before they arise.
Be proactive about how to handle sexual attention, too, possibly from upperclassmen. This can be a particular issue for girls, but any teen should know how to recognize when someone, especially someone older, is making them uncomfortable. “I often talk to young girls about the potential feeling of obligation. Feeling like you have to say like, ‘Oh, that was nice,’ or even smile,” says Janine Domingues, PhD, a senior psychologist at the Child Mind Institute. This kind of attention can feel good, Dr. Domingues acknowledges. But girls shouldn’t feel like they have to reciprocate.
Bottom line: no teen is too old to be reminded to speak up for their personal boundaries.
Managing time — and sleep
While embracing activities outside of schoolwork is important, take it slow. “There’s a lot of time management confusion when you get to high school,” says Klorfein. “Like, I have friends, I have this internship, I have school, and I don’t know how to manage it all.”
Where there is the teen who resists joining any club, there is also the teen who joins all of them. If that sounds like your kid, strongly caution them against taking on more than they can handle. Advise picking one activity and seeing how they handle it with their courseload before adding more.
As much as Ralph loves the soccer team, it has made his academic life much more challenging. “Sometimes he doesn’t get home til like 10pm. And then he has to do homework,” Wendy says. “There have been many, many nights where he’s been up until 1am finishing work.”
And then waking up at 6am for school the next day. Most high schoolers in the United States (nearly 80 percent in 2023) don’t get enough sleep, which can undermine both their performance in school and their mental health. You can’t change what time your teen’s school starts but you can help them develop healthy sleeping habits (no screens in bed) to protect whatever sleep they can get.
Building self-advocacy skills
In high school, personal responsibility isn’t just about staying on top of your schoolwork — it’s about knowing how to speak up when you need something.
This is especially important for students with learning challenges. Make sure your teen identifies at least one adult at school they can reach out to for extra help. And if they need accommodations that they aren’t getting, practice language they can use to ask for them.
When students know how to ask for what they need, they may be more likely to ask for help if they’re having social or emotional issues as well. If a student is struggling emotionally or socially, but also doing well in school, they aren’t likely to come to the attention of school psychologists and other support staff, notes Ashley Cameron, a New York City school counselor. “If you don’t know how to ask for that help, a lot of times it goes unnoticed.” she says. So, make sure your teen knows an adult at the school they can go to for help outside of academics, too.
Why you should stay involved
For parents of high school students, it may be tempting to think that getting involved with larger school community, or even knowing other parents, is no longer important. But Cameron cautions against thinking this way.
“We start to see a huge drop-off of parent involvement at the high school level,” she says. Just attending social events can make a big difference in a teen’s adjustment to high school — which is why Cameron invites the families of incoming freshmen at the high school where she works to an informal community dinner the spring before classes start, in addition to the more formal student orientation. Because as important as it is for you to understand your child’s life at school from their teachers, it works the other way, too.
“Having the school know your student, not only as a student, but as a human and a member of a bigger family — I think that’s important for us as educators to see the bigger picture,” she says.
Frequently Asked Questions
Teens face various challenges when they start high school including mastering new routines, dealing with increased academic pressure, navigating a new social environment, and learning to effectively manage their time.
You can help your teen prepare for their first day of high school by making sure they are comfortable with their commute, understand their school’s entry protocol, and are familiar with their school building so they know how to get to class.
You can help your teen make friends in high school by encouraging them to join an extracurricular club or team. If they struggled to make friends in middle school or were bullied, emphasize high school as an opportunity for them to find their people. They do not have to be an Olympic swimmer or obsessed with photography — the point is for them to meet others who share their interests.
The post Starting High School appeared first on Child Mind Institute.
]]>The post Starting Elementary School appeared first on Child Mind Institute.
]]>Browning has taught kindergarten in Ohio for 11 years, but it still took a few weeks for her daughter to adjust to starting elementary school, and it’s not just the long days. Kindergarten has gotten more academic: In 1998, 31 percent of teachers expected kids to learn to read in kindergarten, while 80 percent did in 2010. Kids might still do fingerpainting and run around on the playground, but they are expected to sit still and do structured activities for the bulk of the day — a big change, even for kids who went to preschool as Browning’s daughter did.
Here are 10 tips from teachers and clinical experts on what you can do to smooth your child’s transition to kindergarten.
Prioritize sleep
“Sleep is so important,” says Kersten Russell, MSEd, a reading specialist on the School and Community Programs team at the Child Mind Institute. “I see a lot of kids who are overtired at school, and lack of sleep can definitely contribute to behavioral challenges or meltdowns.”
Five- and six-year-olds should get 10-13 hours of sleep, according to the American Academy of Pediatrics. Research finds that 5-year-olds who regularly get at least 10 hours transition more successfully to kindergarten, meaning they have higher ratings for behavior, relationships, and academic performance.
Over the summer, you might have let your kid stay up late but try to start adjusting to an earlier bedtime at least two weeks before school starts. “Each day you’re going to make bedtime a little bit closer to the time it’s supposed to be,” says Jane Wong, PsyD, an associate neuropsychologist at the Gund Learning and Diagnostic Center at the Child Mind Institute. You also want to have good sleep hygiene, she says. That means no screens an hour before bedtime and doing a relaxing activity, like reading books together, to help wind down and get sleepy.
Introduce group activities
If kids haven’t been in preschool or day care, it’s helpful to expose them to other structured activities so they can practice following directions from a teacher in a group setting. Otherwise, “they don’t quite understand that they have to sit and listen. Even if they don’t 100 percent want to participate in an activity, they still need to do what everyone else is doing,” Browning says. Russell suggests bringing your child to library story hour or music classes, which are similar to a classroom environment and can go a long way in easing the transition.
Visit the school in advance
“The best thing for parents to do to prepare kids is give them as much predictability as possible,” Dr. Wong says. The actual first day of school can be chaotic, so you don’t want that to be the first time they go there. Bring the child to the neighborhood around school and walk around, making them feel safe, and explain that this is the school they’ll be going to soon. “The tone of voice when you talk to the child is also important, conveying that this is a safe place, a fun place,” she says.
Even kids who have been in a preschool program might get nervous about going to a new school, getting to know an unfamiliar teacher and making friends. It can help if you talk about what might be different in kindergarten to prepare them, Dr. Wong says. There will likely be more kids in the class than in preschool, for example, and older kids in the hallway.
Bring a family photo to soothe anxiety
Separation anxiety is mostly a problem in the first few weeks of school. But it can come up throughout the year after a long weekend or vacation — even with kids who didn’t have problems when school first started.
If kids struggle with separation anxiety, having a photo of their parents or a special trinket with them can be helpful, Browning says. When they feel anxious, they can look at the photo or touch the trinket that their mom and dad had touched before, and that can soothe them. Her school has a therapy dog that also helps calm kids down.
One thing Browning warns against is keeping kids home from school to give them a break or telling kids that if they are having a bad day, they can tell the teacher and the parent will come get them. “If you give kids an option to go home, they’ll reach for that immediately instead of trying to cope,” Browning says.
Normalize feeling nervous
Some kids don’t know any of the others in the class and worry that they won’t make friends. On the first day of school, Browning says, she’ll tell her students, “We are all in the same boat — I don’t know any of you, so I understand feeling nervous.” Parents can say they’re nervous, too, to normalize the emotion.
It can also help to give them a script they can use for meeting someone for the first time. “You can say, ‘Hello, my name is John. Nice to meet you.’ Role-playing can really help,” Dr. Wong says. For kids who have social anxiety, you can practice smiling and waving — “give them as many tools in their toolbox as you can, for whatever they feel comfortable doing.”
Deep breathing exercises can also help kids find calm when they feel anxious. Parents can find belly breathing videos online to watch with their kids and practice together (here’s one with instructions and another on how to use it). The videos show in a very visualized way how to take slow, deep breaths in their belly, like a balloon, and letting it out again. “I suggest following along with the videos because it allows your child to watch and listen to the instructions while they learn and practice belly breathing, and pairing different sensory modalities is important for learning,” Dr. Wong says.
Prepare for potty independence
Don’t be surprised if kids regress a bit at the start of school — having accidents after they’ve been potty trained for years. Kids need to learn to recognize the urge to use the bathroom without being asked by a parent, which takes practice. Another issue is that kids might be used to having parents help them in the bathroom. “Even with my own kids, I didn’t realize that I was going in and doing everything for them,” Browning says. “And then I thought, ‘Wait a second. When I stop doing this, they’re not going to know how to do it.’”
She says it’s important to break things down into small steps and narrate as you go, like remembering to use soap to wash your hands and then getting a paper towel to dry them. “You need to practice until they can do it independently, without prompting,” she says. Otherwise, at school, they will be waiting for verbal prompts from an adult for each step — something the teacher can’t do for every child.
Create a visual checklist
Kids are responsible for their own things at schools, so it’s helpful to practice some of the routines at home before school starts, Dr. Wong says. When they go into the classroom, they will be expected to put their things away in a cubby. “At home, you can pretend. This is your cubby. What do you do when you’re going to the classroom? You put away your jacket, put away your backpack, and maybe take out your water bottle,” she says. Kids can learn to pack their backpack using a visual checklist, with small photos or simple icons of a water bottle, snack, and lunchbox (which you can find on Google Image), for example. These practice sessions are especially helpful for kids who have problems with organization or trouble managing their belongings, she says.
Work on hand strength
In the last few years, Browning has noticed a decrease in fine-motor skills in new students, which translates into trouble with handwriting (she attributes it to the use of touchscreens and tablets supplanting drawing and other play that requires dexterity). If your kids like to use Play-Doh, she says, try substituting putty, which is a little harder to manipulate and will strengthen fingers. She also encourages beading bracelets, threading beads on pipe cleaners, and picking up things with tweezers or a clothespin — anything that will increase dexterity and hand strength. It also helps if kids come in with at least some experience using scissors safely, even if it’s just cutting a piece of paper in half.
Practice opening snacks
If your child has favorite snacks they will want to bring to school, make sure they know how to open them on their own. Parents often twist open applesauce pouches before handing them over to their child, for example, but teachers don’t have time to do that for every kid. With a little practice, little fingers can do it, along with opening zippered baggies and other snacks.
Clementines are another kid favorite — and Browning suggests (on behalf of all kindergarten teachers) that you break open the peel in one spot before putting it in the bag. Start it for them, she says, and kids can usually peel the rest on their own.
Alleviate lunchroom anxiety
Eating lunch on their own is a common worry for kids. In the weeks leading up to school, Browning recommends packing a lunch box and having them eat it at the kitchen table. You can see what they struggle with, so you can practice with them until they feel more confident doing it on their own.
The noise and hubbub of the cafeteria can be tough for some kids, she says, but exposure helps. Take them to a busy food court for a meal so they can get used to eating in a loud place.
Kids can also feel nervous about the lunchroom because they don’t know what to do when they need help. “Before school started my daughter asked me, what if I can’t find my teacher?” Browning says. “She was hung up on the idea that her teacher was the only person she could turn to.” If she got lost finding her way back to the cafeteria from the bathroom, for example, she could go to any adult in the school and ask for help. Telling her daughter that helped alleviate some of her anxiety.
And hopefully, this will alleviate some of your own anxiety as well. You will need to respond to things as they arise but just being aware of what the issues might be can make the transition to kindergarten go a little smoother.
Frequently Asked Questions
- Start with early bedtimes, practice independence (like opening snacks and using the bathroom alone), and visit the school ahead of time so it feels familiar and safe.
Normalize the anxiety by sharing that even adults feel that way sometimes, and practice calming strategies like deep breathing or role-playing how to meet new friends.
Teachers work hard to create a warm, structured environment where kids feel safe and supported — they know most kids are adjusting and are ready to guide them through it.
The post Starting Elementary School appeared first on Child Mind Institute.
]]>The post Early Signs of Bipolar Disorder in Teens appeared first on Child Mind Institute.
]]>Why try to spot these early signs? Because helping kids before the disorder disrupts their lives can actually delay onset and reduce the severity of the disorder. “The earlier we can intervene, the better the outcome,” says Anna Van Meter, PhD, a clinical psychologist and researcher at the NYU Child Study Center.
Full-blown bipolar disorder causes extreme changes in mood, energy, and behavior — periods of feeling unusually happy, irritable, or energetic (mania), followed by times of deep sadness, fatigue, or withdrawal (depression). Until relatively recently, little was known about how to identify the symptoms that came before the first manic or depressive episode.
“Ten years ago, we didn’t talk about the bipolar prodrome,” says Dr. Van Meter. “Now, we’re studying it, we’re developing interventions, and we’re helping families earlier. That’s huge.”
What is the bipolar prodrome?
Think of the prodrome as the “early signs” phase. It’s a period when a young person might be showing hints of bipolar disorder, but they don’t yet meet the full criteria for a manic or depressive episode. Dr. Van Meter puts it this way: “The bipolar prodrome is a time when kids or teens might have changes in energy, mood, or thinking, but it’s not enough to qualify as a full mood episode. These changes might seem small or fleeting, but they’re important to notice.”
Most of the time, these early signs show up in adolescents, though they can sometimes start even earlier. “Bipolar disorder is really uncommon in young children,” Dr. Van Meter explains. “But by the time kids hit puberty, we start to see more signs — especially in those with a family history. We know that bipolar disorder is a very heritable illness.”
She also emphasizes that it’s not just about recognizing individual symptoms but the way they evolve over time: “We’re not just looking for one behavior that stands out — we’re looking for patterns across weeks or months that don’t quite add up. That’s where the prodrome hides.”
What early signs should parents watch for?
What makes the prodrome especially challenging is how sneaky it can be — the symptoms tend to be subtle and easy to chalk up to typical teen moodiness or stress.
Here are some of the most common signs:
- Changes in energy: More hyper than usual or suddenly low energy
- Sleep issues: Trouble falling asleep or needing less sleep without feeling tired
- Mood shifts: Periods of high excitement or irritability that don’t quite cross into mania
- Changes in speech: Talking more or faster than usual
- Changes in concentration: Being easily distracted or having racing thoughts
The prodrome can be hard to notice if you’re not looking for it. “It starts slowly,” says Dr. Van Meter. “Maybe your kid is sleeping less or seems more energized at night. Maybe they’re talking more or acting impulsively. These little changes add up.” Dr. Van Meter encourages parents to trust their gut. “Parents know their kids best. If something feels off — even if you can’t put your finger on it — trust that instinct and start tracking.”
Why are early signs hard to detect?
One word: overlap. A lot of the early symptoms of bipolar disorder look like other things — or just normal teen ups and downs.
Puberty also plays a big role in complicating diagnosis: “Hormonal changes can mimic mood symptoms,” says Dr. VanMeter, “and that makes it even harder to separate what’s clinical from what’s developmental.”
Family history can be a big clue. “If a parent or sibling has bipolar disorder, we pay extra attention to things like mood changes, energy shifts, or impulsivity,” she adds. “It doesn’t mean a child will develop bipolar disorder, but it raises the level of concern.”
Why early detection matters
Spotting signs early isn’t just about slapping a label on a child. It’s about getting ahead of the curve and helping kids before they are in crisis. Reducing stress and targeting good nutrition and, most important, consistent sleep can help delay the onset of illness — a run of not sleeping can actually trigger an episode of mania. “We can teach families how to manage stress, support healthy sleep, and notice when things might be heading in the wrong direction,” says Dr. Van Meter. “That can make a big difference.”
Research also supports the “kindling” theory — the idea that the more mood episodes someone has, the more likely they are to keep having them. “If we can help a young person avoid or delay their first full episode, that could really change the course of the illness,” she adds. Dr. Van Meter emphasizes the role of resilience, too. “We’re trying to build a buffer, help kids develop emotional tools before they’re in crisis. That’s not just preventive; it’s empowering.”
What treatments help?
Here’s the good news: There are effective treatments that can help during the prodrome — even before a child, usually a teenager, has been officially diagnosed with bipolar disorder. Psychoeducation is often the first step. “That means helping the child and their family understand what’s happening,” Dr. Van Meter explains. “We talk about symptoms, stress, sleep, and how to spot warning signs.” From there, many families benefit from therapy, especially family-based approaches. Some of the best evidence-supported options include:
- Family-Focused Therapy (FFT): Helps families communicate better, reduce conflict, and build routines
- Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on building stable daily rhythms (like sleep, meals, and activities) to regulate mood
- Dialectical Behavior Therapy (DBT): Teaches emotion-regulation skills, which can be really helpful for teens dealing with intense mood swings
“We’re not necessarily trying to stop bipolar disorder from developing,” says Dr. Van Meter. “But we are trying to reduce the impact and help the child build skills early.” She also highlights the importance of tailoring therapy to the individual. “There’s no one-size-fits-all approach. We want to match the intervention to the child’s needs — and that takes ongoing monitoring.”
What about medication?
Medication isn’t always the go-to during the prodromal phase — and that surprises a lot of parents. Often, families expect that a prescription will be the first line of defense. But doctors typically start with therapy, education, and lifestyle changes instead, especially if symptoms aren’t severe yet.
Many parents ask, “Shouldn’t we be doing more?” But early on, building good habits and strong communication can be just as powerful — if not more so — than medication. In fact, medication is usually reserved for more severe symptoms or situations where safety is a concern. “If a teen is really struggling — if they’re showing clear signs of mania or severe depression — then yes, we might consider medication,” Dr. Van Meter says. “But for kids who are just beginning to show signs, we usually start with therapy and lifestyle changes.”
When meds are used, doctors might prescribe mood stabilizers like lithium or certain antipsychotics. But every case is different, and it’s important that decisions are made by a child psychiatrist who understands bipolar disorder in youth. Dr. Van Meter advises families to stay involved. “Parents should be part of the treatment conversation from day one. Meds can help, but they’re not magic — they work best when paired with structure and support.”
Can technology help?
It turns out there’s a silver lining to all that time your teen spends on their phone. Dr. Van Meter and her team are studying ways to use technology to catch mood shifts before they become full-blown episodes. The technology picks up on subtle changes in behavior before anyone notices them out loud. The new technology actually helps us understand mental health in real time — and for many parents, that kind of early heads-up could feel like a lifesaver. “We use something called digital phenotyping,” Dr. Van Meter explains. “Basically, we track data from a teen’s smartphone to look for changes in behavior. Are they sleeping less? Are they moving around less? Are they staying home more than usual? These little shifts can tell us a lot.”
The goal is to build a personalized “baseline” for each teen, then flag when things deviate. “It’s kind of like a Fitbit for mental health,” she says. “We’re not there yet, but the hope is that someday we can use this data to give families and clinicians a heads-up before a crisis. We’re trying to shift from reactive care to proactive care. Technology is one of the tools that can help us get there.”
What can parents do to help?
If you’re a parent worried about your child, the most important thing is to stay curious, stay connected, and don’t panic. Dr. Van Meter offers this advice:
- Learn the signs: “The more you understand about bipolar disorder and the prodrome, the better prepared you’ll be.”
- Track patterns: “Keep a simple mood and sleep journal. It helps you and your child see trends over time.”
- Prioritize sleep: “Sleep is huge. Even small disruptions can trigger mood changes.”
- Be open and supportive: “Kids do best when they feel heard and not judged. Keep the conversation going.”
- Find the right help: “Look for therapists or psychiatrists who understand early bipolar signs. You want someone who knows what to watch for.”
And finally: “Don’t wait for a full-blown episode to act,” Dr. Van Meter urges. “If you notice changes, talk to your child, track what you see, and connect with a professional. That early action can really change the trajectory. Early support doesn’t just reduce suffering — it builds confidence. It shows kids they’re not alone and that help is available.”
Frequently Asked Questions
Early symptoms of bipolar disorder include changes in energy level (more hyper than usual or suddenly low energy), needing less sleep, periods of high excitement or irritability, talking faster than usual, and having racing thoughts.
Signs that someone is developing bipolar disorder include being more hyper than usual, needing less sleep, periods of being highly excited or irritable, and talking faster than usual.
Early bipolar symptoms start slowly and can look like other things — or just normal teen ups and downs. Maybe the teen is sleeping less or seems more energized at night. Maybe they’re talking more or acting impulsively. These little changes add up.
Treatment cannot prevent someone from developing bipolar disorder, but it can delay onset and significantly reduce the severity of symptoms. Therapy involves working with the child and the family to help them understand what is happening, how to spot warning signs, and reduce the stressors that can trigger an episode. Evidence-supported therapies include Family-Focused Therapy (FFT), Interpersonal and Social Rhythm Therapy (IPSRT), and Dialectical Behavior Therapy (DBT).
The post Early Signs of Bipolar Disorder in Teens appeared first on Child Mind Institute.
]]>The post Why Reproducible fMRI Is the Key to the Future of Mental Health appeared first on Child Mind Institute.
]]>In a wide-ranging conversation with Peter Bandettini on the Neurosalience podcast, Michael P. Milham, MD, PhD shares a vision for how brain imaging can move from exploratory research into real-world clinical impact.
Dr. Milham, Chief Science Officer at the Child Mind Institute, describes the need for large-scale, open-access neuroimaging data, like those pioneered in the ADHD-200 and Healthy Brain Network initiatives, to capture the true diversity of the human brain. He stresses that reliability, not novelty, is now the field’s central challenge. Variability across processing pipelines threatens progress unless we commit to rigorous standards and transparency.
The conversation explores how deep phenotyping, AI, and real-world data streams (from wearables to electronic health records) can help move the field toward individualized insights—shifting away from group averages to tools that clinicians can trust at the person level.
The take-home message? The future of brain health lies in radical collaboration, open data, and methodological rigor.
Explore Our Open Datasets
- https://fcon_1000.projects.nitrc.org/indi/cmi_healthy_brain_network/
- https://fcon_1000.projects.nitrc.org
The post Why Reproducible fMRI Is the Key to the Future of Mental Health appeared first on Child Mind Institute.
]]>The post How Do You Support a Teen Who Is Nervous About Leaving Home? appeared first on Child Mind Institute.
]]>Start with validation
When they share their anxieties with you:
- Pay attention! Put down your phone, make eye contact, and show you are interested.
- Reflect back what you hear. This shows you are listening and want to understand. Avoid a judgmental tone.
- For example, “I hear you saying you’re worried that you’re not going to know anyone in any of your classes, so you’ll feel isolated.”
- Look for what they’re NOT saying. Check their facial expression, tone of voice, and body language. Is there something they’re afraid to say? Say what you think they may be leaving unsaid.
- For example, “I’m wondering if you’re also worried that you’ll miss your friends and family?”
- Put it in context. Why does it make sense that your child is feeling what they’re feeling? What parts of their anxieties are reasonable based on the circumstances?
- For example, “I think it makes sense that you feel this way! You’ve known your friends since elementary school, and you’ve never gone that long without them. You also haven’t had to make new friends since new people joined in 9th grade, so you’re out of practice. I would be anxious too!”
- IMPORTANT: When validating, don’t argue the other side yet! Your child may “dig in their heels” or “double down.”
After you’ve validated, look for clues that your child is ready to problem-solve
- They may literally ask, “What should I do?” or say, “Help!”
- But it may be more subtle than that. It might be a shift in their mood or body language.
Then, help them build motivation for problem-solving!
Ask questions instead of telling them what you think.
- For example, “I understand why you’re worried about this. I’m also confident that once you find yourself in those situations, you’ll handle them better than you expect. It’s always scarier before it actually happens.”
- If you try to help with problem-solving and your child goes back to expressing their worries, switch back to validation.
- Lastly, don’t be afraid to remind them that you’ll always be available to support them. They may just need to hear it.
The post How Do You Support a Teen Who Is Nervous About Leaving Home? appeared first on Child Mind Institute.
]]>The post What Do Parents of Students With ADHD or Learning Disorders Need to Know Before Their Kids Go to College? appeared first on Child Mind Institute.
]]>It may be bumpy at first
- Keep in mind that your young adult going off to college is still, essentially, a high school student who needs time and space to figure out how to be independent.
- Many students do not perform as well as they — or you — have been used to at first.
- You need to let them figure it out on their own, even if that means making mistakes.
- Parents, teachers, or tutors may have provided significant scaffolding to these students in high school.
- In many ways, adults may have acted as the student’s prefrontal cortex. Now they have to do it themselves.
The student will now independently need to:
- Go to bed at a reasonable hour.
- Wake up on time.
- Make it to class.
- Keep track of their assignments.
- Plan a study schedule.
- Make use of unstructured time.
- Take their medication (if applicable).
- Make — at least somewhat — nutritious eating choices.
Before they leave for college, start having them practice doing these things on their own if they aren’t already.
Help prepare for this transition early
Teach them life skills and tricks you know for:
- Laundry
- Cleaning
- Budgeting and taxes
- Planning and organization
- How to change a tire or complete minor household repairs
Talk to them about their ADHD or learning disorder
- Help them to understand and accept what they need in order to be able to learn effectively.
- If they had a 504 plan or IEP in high school, go over it with them so they can reflect on the supports they had in place.
- They may be reticent to request accommodations from the office of disabilities at college. You can talk about what supports are necessary, and what they can try on their own.
- In the end, they’ll need to make their own decisions regarding accommodations and how much they tell their professors about their struggles.
- Give them a heads up about the ways in which college will be different.
- Many smart students with ADHD or a learning disorder might not have needed to study much in high school, or could get by with waiting until the last minute to study.
- Sustained effort is practically a requirement for success in college.
- Your student may find that their regular “approach” is ineffective.
- Their first-ever academic problems may be interpreted as a personal failure, which can lead to frustration, anxiety, and depression.
- They may hide their “mistakes” from you, for fear of facing the truth or disappointing you.
- Emphasize that they can and should be honest with you, and that you understand that they may take some time to find their groove.
Be an anchor for your young adult
- As much as you need to give your child space, it’s also important to be there for them.
- Many students are experimenting with independence and life changes, but want home to feel familiar.
- Don’t make any big changes at home without first discussing with them.
- Keep them informed of big life events — you may be tempted to hide something like a family illness until they come home, but this can erode trust and increase anxiety.
- Ask them about their life, not their grades.
- Ask questions about what their professor is like, or what they’re doing in their free time.
- If you focus on their academic performance, they may start dodging calls or keeping the truth from you.
- Try your hardest to wait until they ask for advice before offering it.
Reflect on your own feelings
- Your children might absorb or mirror how you feel about any challenges they face.
- Your child needs you to be positive about their ability to succeed in college, despite their ADHD or learning disorder, and realistic about what they need to do get there. If you’re feeling pessimistic, or feeling guilty about “passing on” those challenges to them, work though those emotions.
- Talk to other parents you trust, talk to a psychologist, or talk to others in a parent group.
- Focus on your child’s strengths and provide positive reinforcement and encouragement for their efforts.
- Be a role model by being transparent with them — honesty goes both ways.
The post What Do Parents of Students With ADHD or Learning Disorders Need to Know Before Their Kids Go to College? appeared first on Child Mind Institute.
]]>The post CBS News: How to help kids thrive during summer break appeared first on Child Mind Institute.
]]>The post CBS News: How to help kids thrive during summer break appeared first on Child Mind Institute.
]]>The post CBS Mornings: Keep Your Kids Busy While Building Healthy Habits appeared first on Child Mind Institute.
]]>In this CBS Mornings interview, Dr. Harold Koplewicz, President of the Child Mind Institute, highlights the importance of keeping a consistent routine during the summer to support children’s mental well-being, especially for those facing mental health challenges. He explains that structure helps children feel more organized and less anxious, suggesting parents establish regular schedules for activities like playtime and bedtime. Dr. Koplewicz also emphasizes the critical role of sleep in managing behavior, particularly for children with ADHD, and advises parents to quickly get back on track if sleep schedules are disrupted. He also encourages teaching kids mindfulness and relaxation techniques, such as belly breathing, which can be valuable tools for their emotional well-being.
The post CBS Mornings: Keep Your Kids Busy While Building Healthy Habits appeared first on Child Mind Institute.
]]>The post Mirror: A Lifeline for LGBTQ+ Teens appeared first on Child Mind Institute.
]]>For many LGBTQ+ teens, growing up isn’t just about figuring out who they are, it’s about surviving environments that may not fully see, support, or accept them. In these moments, having a tool that provides safety, space, and self-reflection isn’t just helpful, it’s essential.
That’s where Mirror comes in. Inspired by the real experiences of youth and grounded in research on mental health, Mirror offers more than just a place to write. It’s a refuge, a sounding board — and sometimes a lifeline.
“Without It, I Wouldn’t Be Here Today: LGBTQ+ Young People’s Experiences in Online Spaces,” a report published by Hopelab, highlights how journaling has been a critical source of emotional sustenance for queer teens, especially when traditional support systems aren’t available. Mirror fills this need, creating a digital space designed with care and safety in mind.
Mirror is designed to support the mental well-being of all teens and young adults, regardless of identity or background. At the same time, it offers particular value for LGBTQ+ youth who may face additional challenges navigating stigma, identity development, or lack of support. The features that make Mirror safe, private, and reflective are especially meaningful for those seeking space to process and grow on their own terms.
Here’s why Mirror matters for LGBTQ+ teens:
A Safe Space That Teens Can Take Anywhere
Mirror offers a password-protected, private space where teens can explore identity, process emotions, and reflect without fear of judgment. “Journaling was the first space I had that felt truly mine,” one teen in the Hopelab report said. Mirror makes that safe space portable and protected, wherever and whenever it’s needed.
Emotional Processing That Promotes Self-Reflection
Mirror is built on the power of expressive writing, which has been shown to ease anxiety, depression, and trauma-related stress (Pennebaker & Chung, 2011). For LGBTQ+ youth facing rejection or stigma, Mirror can be a daily emotional support tool.
Freedom to Explore Identity
Mirror empowers teens to explore who they are through prompts, voice notes, and free-form writing. Whether they are trying out a new name, reflecting on gender, or navigating fluid identities, Mirror supports curiosity and authenticity.
This aligns with Hopelab’s findings that digital tools that honor individual identity can promote autonomy and belonging.
Support Through Coming Out and Life Transitions
Coming out, shifting pronouns, or exploring relationships are all deeply personal processes. Mirror offers space to rehearse conversations, record feelings, or reflect after big moments. “Sometimes I couldn’t say things out loud, but I could write them,” shared one youth. Mirror provides a place for LGBTQ+ youth to journal with voice, video, and writing.
Improving Mental Health With Daily Practice
Journaling is more than venting, it’s a practice that builds mental resilience over time. Research supports this: Smyth et al. (2018) found that regular journaling led to significant reductions in anxiety and improved emotional well-being. Mirror’s gentle reminders, mood tracking, and guided prompts encourage consistency without pressure, helping teens build a healing habit.
A Chronicle of Growth
Every entry in Mirror becomes a record of growth, evidence of resilience, clarity, and change. Looking back, LGBTQ+ youth can see how far they’ve come, even through the most challenging times. Seeing that journey reflected builds self-worth and hope, two things no teen should go without.
Getting Started With Mirror
- Use prompts like “How do I feel in my body today?” or “What do I need to hear right now?”
- Try audio or video journaling if writing feels too hard
- Use mood tracking to connect feelings with experiences
As the Hopelab report reminds us, sometimes a tool like journaling literally saves lives. With Mirror, LGBTQ+ teens have a pocket-sized companion that listens, reflects, and empowers every single day. Download Mirror today!
Download Mirror
Available on the App Store and Google Play Store.
Resources
The Trevor Project is the world’s leading suicide prevention and mental health organization for LGBTQ+ young people. Here are some ways to get in touch with the Trevor Project, 24/7:
- Text START to 678-678. You’ll be connected to a trained counselor and be able to message them privately.
- If you want to speak to a counselor directly and confidentially over the phone, you can call 866-488-7386.
- If you want to chat online, visit TrevorChat.org
References
- Hopelab. (2024). “Without it, I wouldn’t be here today”: LGBTQ+ young people’s experiences in online spaces. https://hopelab.org/stories/without-it-i-wouldnt-be-here
- Pennebaker, J. W., & Chung, C. K. (2011). Expressive writing: Connections to physical and mental health. In H. S. Friedman (Ed.), The Oxford handbook of health psychology (pp. 417–437). Oxford University Press.
- Smyth, J. M., Johnson, J. A., Auer, B. J., Lehman, E., Talamo, G., & Sciamanna, C. N. (2018). Online positive affect journaling in the improvement of mental distress and well-being in general medical patients with elevated anxiety symptoms: A preliminary randomized controlled trial. JMIR Mental Health, 5(4), e11290. https://doi.org/10.2196/11290
The post Mirror: A Lifeline for LGBTQ+ Teens appeared first on Child Mind Institute.
]]>The post How Mirror Helps Keep You Safe: Understanding Our Crisis Detection Features appeared first on Child Mind Institute.
]]>Mental health challenges are on the rise among youth. According to the CDC, more than 1 in 3 high school students experienced persistent feelings of sadness or hopelessness in recent years, and many don’t talk to anyone about it.
Journaling can be a lifeline. It gives young people a safe space to express emotions they may not feel ready to share out loud, where they can privately process and reflect. While journaling can be a powerful tool for self-expression, it can also help you explore deeper emotions like sadness, anxiety, or even hopelessness.
That’s why Mirror includes thoughtful, privacy-conscious crisis detection features. These are designed to quietly watch for signs of acute emotional distress and offer support when it matters most, without judgement.

What Is Crisis Detection?
Crisis detection refers to Mirror’s ability to recognize language in journal entries that may indicate serious emotional distress, such as suicidal thoughts, self-harm, or intense hopelessness.
Our technology does not read or analyze every word you write. Instead, it scans for specific high-risk patterns, to help identify if someone may need additional support.
What Happens?
Many teens experience difficult emotions, but not everyone feels comfortable speaking up about what they’re going through. According to the CDC, nearly 1 in 5 high school students seriously considered committing suicide in the past year, and more than 1 in 10 attempted it. These numbers highlight how important it is to have tools that can identify risk and quietly offer support. That’s where Mirror’s crisis detection features come in.
If our system detects a possible crisis, Mirror gently offers support through resources and prompts to connect with a trusted adult or mental health professional.
You are never forced to take action. You stay in control. Our goal is to meet people with care.
You might see:
- A supportive message checking in with you
- A list of immediate resources, such as the Crisis Text Line, mental health helplines, emergency services, and your support system contacts.
What About Privacy?
Mirror uses secure, on-device screening tools to identify high-risk language, but we do not store or share your journal entries. Your data remains confidential, encrypted, and under your control. You can have safety and privacy.
Built for Care, Not Control
We designed Mirror’s crisis detection features with mental health professionals and real users. Every alert, every prompt, and every check-in are designed to be:
- Non-intrusive
- Non-judgmental
- Optional
We don’t diagnose or intervene without your consent. We designed Mirror’s crisis detection features to remind you that you’re not alone, and help is always nearby.
If you or someone you know is in immediate danger or crisis, please reach out to:
- Crisis Text Line: Text ‘HOME’ to 741741 to connect with a real person, available for free, 24/7
- Suicide and Crisis Lifeline: Call 988 for a free and confidential 24-hour crisis, counseling, and referral line
- 911: Call 911 if you are experiencing an emergency situation
- The Trevor Project: Call or text ‘START’ to 678678 for confidential support for LGBTQ+ young people facing distress, identity questions, or tough situations.
- National Eating Disorders Association Helpline: Call 800-931-2237 for help with eating concerns, body image issues, or disordered eating.
- National Domestic Violence Hotline: Call or text ‘START’ to 88788 to get support if you feel controlled, unsafe, or harmed by a partner or family member.
- RAINN: Confidential support for anyone affected by sexual harm, assault, or abuse. Call 800-656-4673.
Want to know more about how Mirror supports mental health? Explore our features or download the app today to start your journaling journey. Take the first step towards better mental health with Mirror.
Download Mirror
Available on the App Store and Google Play Store.
References
Centers for Disease Control and Prevention. (2023). Youth Risk Behavior Survey Data Summary & Trends Report: 2011–2021. U.S. Department of Health and Human Services. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
More About Mirror
The post How Mirror Helps Keep You Safe: Understanding Our Crisis Detection Features appeared first on Child Mind Institute.
]]>The post Child Mind Institute Joins Rare Impact Fund’s Capacity-Building Workshop appeared first on Child Mind Institute.
]]>Last week, the Child Mind Institute joined nonprofit leaders from around the world for the Rare Impact Fund’s first-ever “Capacity-Building Workshop.” The two-day event took place at Google’s Pier 57 headquarters in New York City.

The key mission of the Rare Impact Fund — founded by recording artist, actress, and philanthropist, Selena Gomez — is to increase access to youth mental health services and education globally. They selected the Child Mind Institute’s School and Community Programs because it embodies one key area of their team’s strategic funding priorities — supporting educators in the early identification and intervention of their students’ mental health challenges.
Taylor Barkee, Director of Programs for School and Community Programs, gathered with leaders who represented 30 different mental health organizations from across five continents. Sessions focused on the challenges nonprofit organizations face and the strategies that help them adapt, connect, and sustain their work.

Harold S. Koplewicz, MD, founding President and Medical Director of the Child Mind Institute, also spoke on a panel alongside clinical psychologist and policy advocate Benjamin F. Miller, PsyD, social impact strategist Jorge Alvarez, and ICONIQ Capital Impact Platform Manager Hayley Mead. They discussed the current mental health landscape and the role philanthropy can play in supporting bold, community-led solutions.
Additional sessions offered frameworks for navigating funding changes, refining strategy, and strengthening storytelling. The workshop also made space for something equally important: rest. The closing community support circle gave participants a moment to reflect, reconnect, and remind each other that well-being isn’t a side note — it’s part of the work.
We’re proud to be part of this global community of care and grateful to the Rare Impact Fund for creating space for honest dialogue, shared learning, and collective progress.
The post Child Mind Institute Joins Rare Impact Fund’s Capacity-Building Workshop appeared first on Child Mind Institute.
]]>The post Child Mind Institute Launches Curious, a Mental Health Research Platform appeared first on Child Mind Institute.
]]>The Child Mind Institute is proud to announce the launch of Curious, a newly reimagined digital platform designed to advance mental health research and improve outcomes for children, adolescents, and their families.
Formerly known as MindLogger, Curious was built to help researchers and clinicians better understand how patients’ thoughts, feelings, and behaviors unfold in everyday life. These insights can lead to more responsive care, more effective interventions, and stronger support systems for families navigating mental health challenges.
Created with support from the National Institute of Mental Health (NIMH) and California’s Youth Behavioral Health Initiative, Curious allows research teams to design and deploy studies with tools that are intuitive, customizable, and secure. Participants can engage with studies through the web and our mobile app, sharing information through surveys, daily check-ins, interventions, and other interactive formats — and researchers receive data that reflects real experiences, captured in real time.
Supporting researchers
Curious was designed to meet the needs of scientists, clinicians, and public health leaders who are working to improve outcomes in mental health.
Whether a team is studying anxiety in teenagers, stress among caregivers, or patient engagement with digital therapy, Curious makes it possible to create tools that are tailored to their specific study and simple for participants to use.
The Curious platform supports a wide range of data collection needs including ecological momentary assessment, behavior tracking, 3D interactive cognitive tasks, and digital interventions. Curious is open source, HIPAA-compliant, and ready to support studies in multiple languages and formats.
Scaling mental health interventions with Northwestern University
A powerful example of Curious in action comes from our partnership with the Lab for Scalable Mental Health at Northwestern University, led by Jessica Schleider, PhD, a leading researcher in adolescent mental health.
The Lab set out to solve a pressing challenge: Deliver brief, research-backed mental health interventions to a broad population of adolescents — efficiently, securely, and at scale.
Existing platforms couldn’t meet all the Lab’s needs. They variously lacked the flexibility to customize interventions, the simplicity needed for wide adoption, or the rigorous privacy protections required for working with sensitive mental health data.
Curious provided the foundation to meet these needs. And what emerged from our collaboration is a scalable toolset for delivering single-session interventions (SSIs) — brief exercises that help young people manage anxiety, stress, and self-doubt in actionable ways.
Working together, we developed a user-friendly, no-code builder that allows the Lab to design and launch interactive digital interventions that are both personalized and private. The builder supports anonymous participation and includes features like downloadable action plans — it also eliminates technical barriers for researchers.
The Lab has since migrated assessments used by more than 50,000 teens onto the Curious platform. With standardized delivery and seamless personalization, they’re now able to expand access to high-quality mental health support across diverse and distributed populations.
This work demonstrates how Curious can help researchers both pilot innovations and bring them to life at scale — with impacts that reach far beyond the lab.
That same scalable infrastructure powered the 10-Minute Challenge, a statewide competition in California that gave students the tools to design their own digital interventions to support healthy technology use — proving how Curious can support innovation from the classroom to the clinic.
Why we call it Curious
We renamed the platform to reflect the values that guide our work. Curiosity is the heart of discovery, and Curious invites questions, welcomes complexity, and encourages exploration. Our goal is to create innovative tools that are grounded in scientific rigor and ethical practice.
You can learn more about Curious, explore our partnerships, or get in touch with our team at gettingcurious.com.
We are proud to offer Curious to nonprofit, academic, and research partners who are working to expand knowledge and improve lives. Together, we can support a future where mental health research is more inclusive, responsive, and impactful.
The post Child Mind Institute Launches Curious, a Mental Health Research Platform appeared first on Child Mind Institute.
]]>The post How Vyvanse Is Different From Other Stimulants appeared first on Child Mind Institute.
]]>How does Vyvanse work?
There are two types of stimulant medications used for ADHD — those based on methylphenidate (Ritalin, for example), and those based on amphetamines (Adderall, for example). Some are short acting, and some are long acting.
Vyvanse is a long-acting amphetamine, but it is different from other ADHD medications because it is something called a prodrug — a kind of medication that isn’t active in your system until it is metabolized.
As a prodrug, Vyvanse has no therapeutic effect in its original form (lisdexamfetamine). After you take Vyvanse, in capsule or chewable form, it is converted in the body into an active drug. Enzymes in the bloodstream remove an amino acid called L-lysine from the Vyvanse molecule, converting it into dextroamphetamine, which is the active stimulant that affects the brain.
Once it is activated, Vyvanse affects the levels of two important brain chemicals, dopamine and norepinephrine, which help regulate attention, impulse control, and hyperactivity.
Because it is a prodrug, it has a more gradual onset than other stimulants, lasts longer, and has smoother control over ADHD symptoms, less likely to have spikes or crashes in the level of chemicals it stimulates in the brain.
Advantages of Vyvanse
As a prodrug, Vyvanse can affect children differently than other stimulants. Depending on the child’s needs, those differences can be advantageous.
Slower activation
Vyvanse works only after it’s been metabolized in the bloodstream, so it takes longer to kick in compared to other stimulants.
“When you take Adderall, usually in a half an hour or so, you’ll start to see the benefit of it,” explains Paul Mitrani, MD, PhD, a child and adolescent psychiatrist at the Child Mind Institute. “But when you take Vyvanse it can take from 90 minutes to two hours for it to be metabolized and start working.”
The delayed onset is good for kids who may have a longer commute to school, Dr. Mitrani adds, because you can time it for when they get to class, saving the benefits for when they are needed most.
Smoother symptom control
Vyvanse can provide a steadier release of medication during the day, with fewer spikes in blood levels, minimizing the highs and lows some children experience with shorter-acting stimulants.
“Sometimes kids can feel like a stimulant is ‘too much’ when it hits their system or have a more abrupt drop off in benefits when it stops working which can result in them feeling ‘off’ or more dysregulated,” explains Dr. Mitrani. “In a lot of kids, Vyvanse tends to be smoother.”
Longer acting
Vyvanse is among the most long-lasting stimulants, remaining active for 10–14 hours.
“With Vyvanse, if you take it at 7:00 in the morning, it’s working by 9:00am, and it can be in your system till like 8:00 or 9:00 at night,” notes Dr. Mitrani.
Less end-of-day irritability
Kids come off the medication less abruptly than they do with other stimulants, making them less likely to get irritable when the medication wears off (sometimes called “rebound”).
“Evenings can sometimes be smoother with Vyvanse, because it’s coming out of their system more gradually,” he adds. “You don’t necessarily have that crash you can have with other stimulants.”
Side effects of Vyvanse
Some children tolerate Vyvanse better than other amphetamines because of its slower onset and smoother, longer release. But that extended duration can result in other side effects.
Decreased appetite
The most common side effect associated with stimulants is appetite suppression, which can be most worrying with longest-acting medications, including Vyvanse.
“If you’re taking just short-acting medications throughout the day, you have breaks where maybe your appetite comes back,” Dr. Mitrani notes. “But when your medication lasts for 10 or more hours, you have a big portion of the day where your appetite may be poor.”
Kids on Vyvanse are encouraged to eat a big breakfast before the effect of the medication kicks in. But depending on the child, that can be challenging, he adds. “Maybe they’re not a breakfast person, or they’re rushing out the door.” Another thing he notes is that sometimes kids with ADHD, when they’re not treated, just can’t sit for a meal. “Treating ADHD can help kids sit better for meals, but now their appetite is gone.”
Some kids are able to catch up with the calories they need in the evening, when the medicine wears off, and suddenly they are starving. But it’s important to monitor their weight, Dr. Mitrani says, to make sure the loss of appetite isn’t interfering with their growth and healthy development.
Trouble sleeping
Difficulty falling or staying asleep is another common side effect of Vyvanse, as it is with other stimulants. Again, the length of time that the medication is active is a challenge — taking it by 7 or 8 in the morning can minimize trouble falling asleep in the evening. Creating a bedtime routine that avoids stimulation can also help. Another possibility is to talk to your doctor about lowering your child’s dose of Vyvanse.
Suppressed mood
“Sometimes kids complain that they don’t feel like themselves on the medication, that their personality is gone, or they feel dulled,” Dr. Mitrani notes. “That is a significant complaint, because we want kids to feel good and do well in school. We don’t want them to be robots. So, if that’s happening, it could be that the dose is too high. Or it could be that the medication isn’t right for them, so we need to adjust.”
Anxiety or jitteriness
When patients report an increase in anxiety, Dr. Mitrani tries to determine whether it’s situational — as in, they’re anxious about specific things — or more general.
“If it’s situational, it could be that the medicine is doing what it’s supposed to do, helping them focus better, but now they’re focusing on things like not getting invited to a party, or a scary movie they saw,” he explains. “If they are more anxious across the board, and feeling more edgy or panicky the entire day, then it suggests that the dose or medication is too much for them.”
As with any medication for ADHD, if your child is trying Vyvanse, it’s important to work with your doctor to find the right dose — one that balances effectiveness with minimizing side effects. And if it turns out that your child doesn’t tolerate it well at a level that’s effective, another medication may be a better fit.
Frequently Asked Questions
Side effects of Vyvanse can include decreased appetite, trouble sleeping, suppressed mood, and increased anxiety or jitteriness. Some kids may feel “off” or unlike themselves if the dose is too high, and appetite loss during the day may impact growth if not monitored.
Vyvanse typically lasts 10 to 14 hours. If taken at 7am, it usually starts working around 9am and can remain active until 8pm or 9pm.
If the Vyvanse dose is too high, kids may feel dull, not like themselves, or emotionally flat. They may also become more anxious or jittery, suggesting the dose or medication may need adjustment.
The post How Vyvanse Is Different From Other Stimulants appeared first on Child Mind Institute.
]]>The post South African and Brazilian Youth Leaders Reimagine Global Mental Health Care appeared first on Child Mind Institute.
]]>South Africa, Brazil — The Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute convened a forum with 31 youth mental health advocates from the South African Federation for Mental Health (SAFMH) and Young Peacebuilders, Brazil.
During the virtual event, which took place on June 17 in celebration of National Youth Day in South Africa, young mental health leaders, spanning ages 14 to 24, presented the different initiatives they are involved in their communities from solution-focused models of advocacy, integration of mental health care in schools, and advisory mechanisms to strengthen systems and influence policy change in Brazil and South Africa.
Eduardo Vasconcelos, director of youth engagement at the Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute, said striking parallels were revealed during the dialogue — particularly related to stigma — while unique cultural approaches and community resilience were also highlighted for their capacity to accelerate transformation.
“True safety is built through empathy, community, and trust, and that only happens when students are not just part of the conversation but at the center of it. That’s how Young Peacebuilders, Brazil, was born,” said Anna Laura Praxedes, the 18-year-old director of operations at Young Peacebuilders, Brazil, a participant of the forum.
Young Peacebuilders, Brazil, empowers students to promote a culture of peace in the school environment through dialogue, empathy, and leadership. Through a unique partnership with the Ministry of Education, they are transforming schools into welcoming and inclusive spaces, where conflicts are resolved collaboratively and where respect and diversity are valued. Their methods focus on building skills that help reduce anxiety — including breathing, movement, and meditation techniques — as well as innovative participatory processes that make teaching professionals active participants and multipliers for peace in their schools.
In South Africa, as in many places around the world, young people have faced exclusion from important mental health policy and decision-making spaces, resulting in policies and practices being developed without their voices included. To change that, SAFMH, an SNF Global Center partner, piloted the first-of-its-kind national youth advocacy and advisory forum for mental health.
“I joined the South Africa Federation for Mental Health Youth Forum because I’ve seen how mental health struggles affect so many young people — for my university friends, in my community, and even in my own life,” said 23-year-old Angel Mdluli at the forum. “So many of us don’t talk about it because we are scared of the stigma, and sometimes we don’t know where to go for help. So, I wanted to be part of something that creates real change.”
During the forum, many commonalities arose. Youth leaders from Brazil shared with their colleagues in South Africa tips on how to get buy-in from school leadership, and youth leaders from South Africa shared with their new colleagues from Brazil how to write memos and policy briefs for government stakeholders. Both groups shared challenges they face in integrating racism and sexism into conversations around mental health. They had very important conversations around the skills necessary to take care of oneself in order to be a leader in the mental health space. These cross-cultural dialogues are an invaluable way to share learnings and insights for the next generation of mental health leaders and an important part of the SNF Global Center’s work.
“The SNF Global Center continues to be in awe of incredible young advocates committed to engineering evidence-informed, scalable solutions that reimagine mental health care understanding and delivery. We are honored to have led this meaningful connection between Brazil and South Africa,” Vasconcelos said. “By partnering with children and adolescents and positioning them as primary architects of equitable, quality, and culturally attuned mental health care reform, this dialogue session transcended traditional models.”
The SNF Global Center continues to lead and support cross-cultural partnerships and elevate youth-driven solutions that authentically reflect the needs of diverse communities, which have been historically underrepresented.
About the SNF Global Center at the Child Mind Institute
The SNF Global Center brings together the Child Mind Institute’s expertise as a leading independent nonprofit in children’s mental health and the Stavros Niarchos Foundation’s (SNF) deep commitment to supporting collaborative projects to improve access to quality health care worldwide. The center is building partnerships to drive advances in under-researched areas of children and adolescents’ mental health and expand access to culturally appropriate training, resources, and treatment in low- and middle-income countries. This work is conducted by the Child Mind Institute with support from SNF through its Global Health Initiative (GHI).
About the Child Mind Institute
The Child Mind Institute is dedicated to transforming the lives of children and families struggling with mental health and learning disorders by giving them the help they need. We’ve become the leading independent nonprofit in children’s mental health by providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing tomorrow’s breakthrough treatments.
About the South African Federation for Mental Health
The South African Federation for Mental Health (SAFMH) is a leading nonprofit, nongovernmental organization committed to advancing mental health and well-being across South Africa. Founded in 1920, SAFMH works to ensure equitable access to quality mental health care, with a focus on serving vulnerable and under-resourced communities.
About the Young Peacebuilders, Brazil
Young Peacebuilders, Brazil (Jovens Líderes pela Paz) is a youth-driven initiative that empowers students to foster a culture of peace within school environments through dialogue, empathy, and leadership. The program aims to transform schools into inclusive and welcoming spaces where conflicts are resolved collaboratively and diversity is embraced. Believing in the power of youth as agents of social transformation, the initiative provides young leaders with the tools and support they need to inspire positive change in their communities.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post South African and Brazilian Youth Leaders Reimagine Global Mental Health Care appeared first on Child Mind Institute.
]]>The post Assessing Nonverbal and Minimally Verbal Children appeared first on Child Mind Institute.
]]>Some children might have autism spectrum disorder, intellectual developmental disorder, language disorder, speech-sound disorder, or apraxia of speech — so it’s important to get a child evaluated by a clinician to get the proper diagnosis.
When a child can’t speak to respond to questions, it’s more difficult for clinicians to assess cognitive functioning and give a diagnosis — but it’s not impossible. Also, there are good reasons to get evaluations done for nonverbal children every few years, to make sure the interventions and treatments are at the right level as they grow and respond to supports.
What does it mean to be nonverbal or minimally verbal?
All children under the age of 18 months speak few words, so kids who don’t speak at that age are considered preverbal. Researchers consider a child over 18 months who doesn’t speak any words to be nonverbal. Kids who can say significantly fewer words than expected for their age are considered minimally verbal. For example, a child who is 30 months or older and can speak fewer than 50 words is below the 10th percentile and would be minimally verbal.
Babies who are preverbal just haven’t developed the ability to speak yet. Young kids who are nonverbal might still develop the ability to speak with time and therapy. Indeed, in one study of kids with autism who were minimally verbal at age 4, 70 percent went on to develop the ability to communicate in phrases or fluent speech by age 8.
But some children will remain nonverbal or minimally verbal through adulthood, and it is important not to let their lack of language get in the way of understanding and addressing their needs, says Daryaneh Badaly, PhD, ABPP, a clinical neuropsychologist.
Language and neurodevelopment
While some children may not speak because of motor mechanism issues, language delays are thought to be related to differences in brain development. When neural development is so severely impacted that a child is nonverbal or minimally verbal, there is a higher likelihood that they also have other neurodevelopmental conditions, such as autism spectrum disorder or intellectual disability.
Kids with autism are impaired in their social communication skills and have restricted or repetitive behaviors and interests. Intellectual disability involves limitations in reasoning, problem-solving, and decision-making skills as well as in adaptive skills (abilities to function in daily life).
Evaluating for conditions such as autism and intellectual disability helps figure out the broader spectrum of a child’s needs, but it doesn’t always get done in young children. In particular, assessments for intellectual disability can be delayed in children with reduced language skills.
It may seem like cognitive testing is not feasible until a child can use language to follow directions and respond to prompts. However, that is not the case. Cognitive testing is still possible with nonverbal and minimally verbal kids.
For example, tests of nonverbal intelligence, combined with background information from parents and others in a child’s life, can help understand if a child meets criteria for intellectual disability. Tests with no (or minimal) language demands can also help to evaluate children’s attention, inhibitory control, visuospatial skills, and learning and memory.
Importance of evaluations for nonverbal or minimally verbal kids
Evaluations help families understand where the child stands and what might be most useful at that moment, Dr. Badaly says. Too often, she finds that families bringing in an older child don’t have a complete view of their child’s functioning.
Understanding a child holistically means that you can help tailor their education to meet their academic and adaptive needs in way that not only maximizes their skills but reduces frustration, she says. “If a lesson is too far beyond what a child can do, they will disengage and get upset,” she explains. “If it is too far below their ability level, they will get bored and miss out on the opportunity for further skill development.”
Even if focusing on verbal fluency is not the right goal for a child, improving their communication might be. “We might want to focus more on adaptive skills,” Dr. Badaly says. “We might aim to get them 10 extra words they can express, gestures they can use, or visuals they can designate, because that’s going to put them in a better position to stay safe.”
Types of assessments for nonverbal children
Most tests require kids to understand directions and give a verbal response, but there are several assessments that clinicians can use for nonverbal and minimally verbal children. To determine if a child meets criteria for autism, for example, the Autism Diagnostic Observational Scale, Second Edition (ADOS-2), includes modules for children who are preverbal or have single words as well as those who speak fluently. In addition, structured interviews with parents can provide rich information on social and behavioral adjustment.
Clinicians will look for other signs that a child is socially engaged even if they have limited language, Dr. Badaly says: “They might smile and wave to others in greeting, use their eye gaze to get and direct others’ attention, attempt to play with others, and share their toys.” Those signs would indicate a child has developed social communication skills even if they are limited in oral expressive language. Clinicians will also look for signs of restrictive and repetitive behaviors and interests that would suggest of concerns beyond the impact of limited language skills. Examples might be stereotyped behaviors such as spinning in circles and highly focused interests such as watching the same cartoon over and over.
Similarly, observations and reports from families and others in a child’s life can help understand if a child meets criteria for attention-deficit hyperactivity disorder (ADHD).
Some nonverbal kids cannot speak but can understand oral language. Others have very limited comprehension of spoken instructions, which makes assessments of intelligence more difficult. For those children, clinicians can use mimed instructions with the Leiter International Performance Scale (for children ages 3 and up), for example.
Even if a child has few spoken words, understanding what they grasp of language is important. Clinicians might assess a child’s understanding of language by testing their vocabulary or understanding of sentences, having them point or tap a picture on an iPad to give an answer. Some examples of receptive vocabulary measures include the Peabody Picture Vocabulary Test, Fourth Edition, or the Ortiz Picture Vocabulary Acquisition Test, the latter of which has a scoring system that look at expectations for children from either monolingual or bi/multilingual homes.
Clinicians will also ask other people in the child’s life, especially parents, to give input on their ability to communicate. “We’ll use something called the Communications Matrix, for instance, which goes from the first levels of communication that you’re gaining typically in your first month of life and forward,” Dr. Badaly says. “For example, can they intentionally ask for something? If so, then how are they asking? Are they dragging your hand? Can they point to it? Are they using eye contact?” Such tools can give a better description of a child’s means of communication to then help their educators and service providers work with them.
Next steps after an evaluation
Getting a fuller picture of a minimally verbal child’s abilities can help clinicians and families figure out what would be most helpful.
“Let’s take a family for whom the whole focus was on language ability, and maybe the child’s autism was missed,” Dr. Badaly explains. “Now, with an autism diagnosis, we’re in a position where we can better understand some of the behavioral struggles that the child has.” It might have been assumed that the child had behavioral challenges because they could not speak. While that may be part of the story, they may also be overwhelmed by the sensory stimulation in their environment and struggle to deal with changes — factors that can be addressed with different strategies. “You might have this gut feeling as a parent that your child needs something different, but you don’t have anything to back that up,” says Dr. Badaly. “An assessment helps give you guidance to figure out what’s needed.”
Frequently Asked Questions
A child over the age of 18 months who doesn’t speak any words is considered nonverbal. Minimally verbal children can speak significantly fewer words than expected for their age — for example, a child over the age of 30 months who speaks fewer than 50 words.
It is typical for children under 18 months to be preverbal, meaning they haven’t developed spoken language yet. However, if a child over 18 months has no words or very limited verbal ability, they should be evaluated by a professional.
Most tests require kids to understand directions and give a verbal response, but there are several assessments that clinicians can use for nonverbal and minimally verbal children. To determine if a child meets criteria for autism, for example, the Autism Diagnostic Observational Scale, Second Edition (ADOS-2), includes modules for children who are preverbal or have single words as well as those who speak fluently.
The post Assessing Nonverbal and Minimally Verbal Children appeared first on Child Mind Institute.
]]>The post Medium: Understanding ADHD: A Comprehensive Guide to Supporting Your Child’s Development appeared first on Child Mind Institute.
]]>Play-based activities support the healthy development of preschoolers and allow them to experience the positive emotions that are essential for their well-being. When preschoolers pretend to play as their favorite characters, it gives parents and caregivers a natural ‘in’ to play along with them and brings joy to the whole family,” said Kathryn L. Keough, Ph.D., clinical psychologist at the Child Mind Institute.
The post Medium: Understanding ADHD: A Comprehensive Guide to Supporting Your Child’s Development appeared first on Child Mind Institute.
]]>The post Collaborative Solutions: Cross-Sector Partnerships Transforming Mental Health Data Systems Across Cultures appeared first on Child Mind Institute.
]]>
By Giovanni Abrahão Salum, MD, PhD
Vice-President, Global Programs, Child Mind Institute
&
Antonis Kousoulis, MD, MSc, DrPH
Director of Partnerships at United for Global Mental Health & Secretariat Lead of the Global Mental Health Action Network
Every two seconds someone under the age of 70 dies from one of the noncommunicable diseases that are the leading causes of death, morbidity, and disability globally. Mental health conditions now account for a staggering 16 percent of the noncommunicable diseases (NCDs) burden, with disproportionate impacts on young people living in low- and middle-income countries (LMICs). This global crisis requires an immediate shift beyond traditional healthcare systems, one that catalyzes cross-sector partnerships, youth-powered solutions, and targeted interventions that are effective across cultures. Due to the social and economic consequences at stake, this issue requires a reordering of global health priorities at the national and subnational levels and scaling up investment into the mental health sector.

Humanitarian imperative
New research projects that expand mental health interventions could contribute USD 4.3 trillion to the global economy and add 57 million people to the global labor force by 2050, representing a humanitarian imperative and major economic opportunity. As we continue to move with urgency and purpose, our cross-sector partnerships model has already yielded transformative results in advocating for and advancing quality youth mental health care, accessibility and reducing the knowledge gap.
The Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute alongside our partners, United for Global Mental Health and the Global Mental Health Action Network, have uncovered staggering gaps in youth mental health care data in LMICs. In addition, we have found that most of the available datasets were collected prior to 2010 and do not reflect our youth’s current needs. Such outdated data is fundamentally disconnected from the real, urgent needs of today’s youth and hampers the ability to make evidence-based policy decisions. The devastating effects of events such as the COVID-19 pandemic, natural disasters, war and conflict, political instability, economic volatility, and systemic underinvestment in youth mental health remain largely uncaptured.
Currently, children and adolescents living in low and middle-income countries are the most negatively affected by mental health data gaps and lack of culturally adapted care and resources. Our joint study, “Data Gaps in Prevalence Rates of Mental Health Conditions Around the World: A Retrospective Analysis of Nationally Representative Data,” recently published in The Lancet Global Health Journal, reveals that the largest documented gaps are in the Western Pacific and Africa. The fragmented data and infrastructure to support those who need care most remain shockingly insufficient.
Without accurate, culturally relevant data informing policy, strengthening systems to improve the mental health landscape is impossible. The alarming consequence is interventions with cascading blind spots where information is incomplete or culturally misaligned.
Sustainable youth mental health initiatives require strengthened coordination and alignment across sectors. This approach is intended to strategically target the complexity of the interconnected layers of youth mental health challenges, including physical and emotional wellbeing, social connections and cultural backgrounds, which are factors that can affect each other and form pieces of the same puzzle.
Innovation through integration: cross-sector mental health solutions
To drive upstream initiatives, we are focused on promoting partnerships across various sectors including education, technology, civil society organizations, the private sector, youth-led organizations, and creative industries, always strongly underpinned by the expertise of lived experience. Each brings a unique perspective on interventions, while ensuring solutions that are effective across cultures and communities.
Our work in transforming children’s lives is centered on cross-sector collaboration that addresses system gaps. Only when we have accurate data can we change how we understand and respond to child and adolescent mental health and see a promising path forward. This includes exploring avenues such as:
- Cross-sector data sharing agreements between education and healthcare systems developed with youth input
- Technology partnerships to analyze mental health trends among young people and AI development
- Joint training initiatives between mental health professionals
- Low-intensity interventions
- Creating innovative funding mechanisms alongside the financial sector
- Partnerships with academic institutions that place youth as co-researchers to revolutionize data collection methods while capturing lived experiences
Another important factor to note within cross-sector partnerships is the adoption of open-science frameworks, which support the transparent sharing of data, protocols, and analytical methods that transcend geographical and institutional boundaries. The above examples are scalable focus areas requiring further development and investment.
Youth as co-leaders: ethical approaches to data practices
The inclusion of youth as partners and co-leaders can transform approaches from well-intentioned interventions to authentic co-creation that addresses both clinical needs and lived experiences. Our work alongside global youth advocates and youth-led organizations has catapulted our efforts in minimizing stigma, unlocking ways of interpreting and disseminating knowledge and data, and creating opportunities for young people to embody their role as active citizens.
Young people are more than just recipients of mental health interventions — they are experts in designing and implementing the programs and services that best address their needs. Their feedback on issues such as participation, data collection, and privacy is instrumental in fostering genuine engagement, improving implementation outcomes, ensuring cultural relevance of assessment tools, and developing ethical frameworks.
Ultimately, youth partnerships and higher participation rates can strengthen entire data systems, enable strategic resource allocation, and improve mental health systems that youth can trust. To ensure effective interventions that match reality, the need to systematically remove barriers through community-led implementation strategies, youth partnership, culturally responsive data collection methods, and adaptable frameworks is critical.
These collaborative methods require expanded cross-sector partnerships and the establishment of a common measurable language that also facilitates meaningful comparisons and harmonization of definitions across diverse cultures and communities. This would also mean institutions such as schools, community organizations, tech companies, and so forth, can create shared ways to talk about and measure youth mental health across different cultural environments. Together, we can identify effective interventions rather than disconnected, standardized approaches.
This will result in higher participation and retention rates, more accurate and up-to-date data, better resource allocation, effective knowledge sharing, and equitable service delivery to underserved communities.
The post Collaborative Solutions: Cross-Sector Partnerships Transforming Mental Health Data Systems Across Cultures appeared first on Child Mind Institute.
]]>The post Reese Witherspoon’s Hello Sunshine Launches Gen Z–Focused Brand Sunnie appeared first on Child Mind Institute.
]]>The post Reese Witherspoon’s Hello Sunshine Launches Gen Z–Focused Brand Sunnie appeared first on Child Mind Institute.
]]>The post Hello Sunshine Launches Sunnie, New Multimedia and Experiential Brand for and by the Next Generation of Storytellers, Creators, and Changemakers appeared first on Child Mind Institute.
]]>The post Hello Sunshine Launches Sunnie, New Multimedia and Experiential Brand for and by the Next Generation of Storytellers, Creators, and Changemakers appeared first on Child Mind Institute.
]]>The post The 5-Minute Daily Bonding Ritual (That Actually Works) appeared first on Child Mind Institute.
]]>- “You matter.”
- “I’m listening.”
- “I enjoy being with you.”
Clinical psychologist Dr. Laura Markham says, “Connection is the foundation of cooperation. Five minutes of connection can prevent 50 minutes of power struggles.”
The post The 5-Minute Daily Bonding Ritual (That Actually Works) appeared first on Child Mind Institute.
]]>The post Screen Time and Summer appeared first on Child Mind Institute.
]]>To make sure that doesn’t happen, it’s important to step back and assess your approach to your kids’ tech use. It’s useful for families to think of a few basic principles when planning a summer screen time strategy.
- Know your risks. What harms do you want to avoid?
- Think about wellness. What do you want your kids to do for their health and well-being over the summer?
- Focus on your values. What will make you feel, at the end of the summer, that your kids have had the experiences you would hope for them?
- Make a practical plan. What concrete steps can you take so you won’t have daily battles over screen time or feel that you are doing something wrong as a parent?
What are the risks?
Because of the intense national conversation about the effect of screens on youth development and mental health, it’s easy to be confused, as a parent, about what to do about screens. Luckily, research has given us some answers. Knowing what the science says about the risks around screens enables you to have a practical, not a panic-based, approach.
Time spent
When considering the amount of time a child or teen spends on screens, the research often refers to a Goldilocks hypothesis: that moderate amounts of screen time may be better than excessive amounts or no time at all. There is definite evidence that spending more than a few hours a day on screens can have a negative effect on a child’s or teen’s well-being — not necessarily because what they’re doing on the screens is intrinsically harmful but because that level of screen activity is interfering with key developmental tasks. Those could include physical exercise, face-to-face time with friends or family, and activities that promote learning. A moderate amount of time spent on screens can be a source of relaxation, entertainment, or social connection, but when screen time becomes excessive, it can displace important daily or social routines.
Solo screen exposure
Not all screen time is created equal. It matters where you spend your time on screens and who you spend it with. Kids watching TV in the living room, kids on tablets or computers in common area of the house — these are less worrisome because we can monitor the sound that’s coming from the screen and perhaps get at least a glimpse of what they are seeing and doing, who they are interacting with, and what content they are being exposed to.
When kids are spending time on screens alone in their rooms, those are more often the instances when they might get into something where a parent later says, “I wish I could roll that back.” It’s important for parents to talk through what you feel is okay for kids to be doing when spending time on screens alone and set boundaries for when you are not present to monitor.
So things like letting kids watch a movie or have some TV time to give you an opportunity to cook dinner shouldn’t be as much of a concern. As much as possible, we want to decrease parental guilt a bit about these kinds of activities, conserving energy for boundary-setting when it is more important.
Video game chat
In previous generations, parents were often concerned about games focused on violence. What kinds of activities are the characters doing, and does playing those games normalize those activities? But the research linking violent games to aggressive behavior on the part of gamers is quite mixed. For parents today, concerns often center less on video game content and more on chat functions and the potential for contact with strangers.
Obviously, we don’t necessarily want young kids to be playing violent video games, but the bigger worry now is the fact that lots of the video games for kids have chat functions that kids don’t understand. These chats, both within and outside of video games, can be a cesspool for cyberbullying, contact with strangers, and predatory behavior. It’s immensely important to teach kids about privacy settings, how to ensure they are connecting with friends and not strangers, and how to reach out for support if they find themselves harassed or bullied in these spaces.
Disturbing content
We want to be mindful of the fact that teens are more likely, no matter when or how they’re spending time on screens, to be exposed to disturbing or offensive content or content that is promoting unhealthy attitudes or practices. With social media algorithms being as sensitive they are, the longer a teen watches a video or peruses certain types of content, the more that content might be pushed to their feeds. Additionally, false information is everywhere online, and it is important that we teach kids and teens to be critical consumers of what they read and watch in an age of AI, conspiracy theories, deepfakes, and more.
Mental health vulnerabilities
One more thing that I emphasize to parents is that if your child has mental health vulnerabilities, the risk factors above are even more deserving of careful consideration. Children and teens with ADHD or behavioral challenges may be less able to avoid impulsive behavior or to set appropriate limits for themselves with screens. Kids who are prone to anxiety may be more likely to seek out content that feeds rather than soothes their worries. And teens who are vulnerable to depression or already experiencing concerns about body image can find that their symptoms worsen when screens cannibalize the time they would have spent on more mood-boosting activities or leave them comparing themselves to unrealistic online body ideals.
So any practical plan we create for the summer involves some monitoring of time, some monitoring of content, some monitoring of behavior online, and some monitoring of where and when kids are on those screens. To build out that plan a bit more, parents can consider a few basic notes on wellness practices and reflect on their own values in seeking family balance this summer.
Promoting wellness
When creating a plan for tech use, we want to make sure that screen time is not encroaching on basic things kids need to be healthy.
Protect sleep
The digital age doesn’t make it easier for anyone — kids or adults — to get the sleep they need. Yes, it’s okay to be a little more relaxed about bedtime during the summer. Yes, kids might sleep in a little bit more than they would if they were going to school. But we want to encourage parents to think about how to make sure kids are getting the amount of sleep they need and that screens are not interfering.
I see a lot of families who dock all devices to charge outside of bedrooms at night, and that is absolutely something I encourage whenever possible with kids and teens. But other parents will say, “My kid uses this to fall asleep. They listen to books on tape or music as they go to sleep.” Or “I want my kid to listen to a meditation or mindfulness recording while they’re going to sleep.” I think that’s perfectly fine as long as we can truly place limits on what a child or teen would have access to past certain hours. And in that case, it can be effective to use an app or screen time limits that lock down anything beyond what might be helpful in promoting sleep.
Prioritize physical activity
Globally, we’re seeing physical activity decrease among youth. There are a variety of reasons for that, and screens aren’t the only driving factor. But the good news is that summer is a great time to catch up. So the other major wellness habit that is good for parents to be thinking about is: How are we making sure that moving their bodies is prioritized over sedentary screen use?
The most straightforward trade-off for kids who might not be attending camps or might not have access to a lot of structured recreational summer experiences is just to reserve a portion of each day for play outside, playdates with peers, walks through the neighborhood, trips to a local park, or even a walk around town to do an errand or two. These can be no-screen times, ideally happening before the portion of the day when kids might be engaged in screen-time activities, with an understanding that moving our bodies should come first. Even if kids need to be indoors on a rainy day or because that’s where an adult can watch them, we can use things like dance videos or guided yoga routines to get kids invested in movement before they might take some time to sit down with screens.
What are your values?
When I ask this question, many parents say that what they value over the summer is unstructured time — opportunities to spend time outside, do enjoyable activities with their kids that they don’t get to do during the school year, or spend more time with neighbors, friends, or family. And when we ask parents what they want their kids to do with that time, we hear parents say they want their kids to explore, to be creative, to maybe be bored a bit of the time, and to have unique experiences.
As kids move into adolescence, parents often say they want to see their teens broaden their interests, invest more in their passions, do community service, gain work experience, or otherwise build character through new experiences. And there there is always that specter of learning loss lurking in parents’ minds — how do we make sure that our kids exercise their brains a bit over the summer in the same way we want them to exercise their muscles?
No parent can do all of the above, so it’s important to reflect on your values and to approach them incrementally (e.g., small steps) and with some self-compassion. Take just one or two of the suggestions above — or your own alternatives — and consider how you might be able to create space for our kids to have these experiences. It’s better to conserve your energy and invest in making moments count than trying to hold yourself to an ideal of parental perfectionism all the time.
Making a practical plan
Many of the non-screen activities parents say they want their kids to do over the summer are done roughly during what would be school hours. So the most frequent times that screens are an issue for parents during the summer often remain the unstructured hours in the afternoon up through bedtime.
If you go through the rough checklist outlined above, you may find it leads to considerably less worry about the time your kids are spending on screens. If you have taken steps to ensure that kids are getting sleep they need, getting their bodies active, and engaging in activities that you see as critical to their summer experiences, then you can feel better about the screen time they are enjoying.
When you have decided what activities you’re okay with, where in the house you’re okay with them, what times of day you’re okay with those things happening, you can take the threat level down and feel a little bit more confident that it’s not the Summer of Screens. This will enable you to give your kids what can be a reasonable dose of screens during the times when you need it most to stay sane, care for yourself, and care for the family as a parent.
Frequently Asked Questions
While screen time can be a source of relaxation and connection, research supports the “Goldilocks hypothesis”: moderate use is best. More than a few hours daily can interfere with crucial developmental activities like exercise, social interaction, and learning. Balance is key — allow some screen time but prioritize off-screen experiences.
Kids prone to anxiety, depression, or behavioral issues may be more affected by screen time. Excess use can displace mood-boosting activities like exercise, socialization, and creative play, and lead to harmful social comparison or exposure to problematic content.
- Protect sleep: Keep screens out of bedrooms overnight or set limits for app usage.
- Prioritize movement: Schedule daily outdoor time, walks, or indoor physical activities like dance or yoga.
- Promote creativity and exploration: Encourage screen-free hobbies and unstructured play.
The post Screen Time and Summer appeared first on Child Mind Institute.
]]>The post Phones Out, Focus In: Crafting Classroom Policies That Work for Everyone appeared first on Child Mind Institute.
]]>By Michael P. Milham, MD, PhD
Chief Science Officer, Child Mind Institute
Across New York and the nation, schools are confronting a complex challenge: the urgent need for learning recovery, a deepening youth mental health crisis fueled in part by unfiltered social media access, and the constant presence of smartphones. Unchecked use of phones not only pulls students out of the classroom moment and negatively impacts learning, but can elevate stress, fuel social tensions, and expose young people to harmful digital dynamics like bullying and toxic comparisons.
The impact of personal devices during the school day demands clearer focus and thoughtful action. Gov. Kathy Hochul’s announcement that New York is banning smartphone use during school hours is a strong first step. How to implement the ban has been left up to individual school districts and that should prompt carefully crafted, individual solutions. A rural middle school and an urban high school face different realities.
That’s why at the Child Mind Institute, we believe limits on personal phone should be developed collaboratively, giving students, parents, educators, and experts a voice in designing an effective strategy for each school — not to demonize devices, but to create classrooms where teachers can teach, students can focus, and healthier tech habits can take root.
What the Evidence Tells Us
The research is compelling. Meta-analyses covering thousands of students reveal that even silent phones nearby can impair working memory and problem-solving. Classroom-level effects are also clear: one distracted student can lower the performance of peers, with boys and students in under-resourced schools often disproportionately affected. Meanwhile, students who most benefit from predictable environments — those who have ADHD, anxiety, or other challenges — find the constant pull of notifications especially disruptive to learning.
Yet the same research reminds us that simply banning phones without guidance misses a crucial opportunity. When schools pair limits with strong digital-literacy programs, students gain the self-management skills they’ll need long after graduation.
Principles for Effective, Equitable Policies
- Local partnership. Policies work best when students, families, educators, clinicians, and administrators co-design them, addressing practical concerns from the start.
- Data-driven, adaptive roll-out. Design pilot programs, measure their impact on learning and school climate, adjust, and scale thoughtfully. Phone policies deserve the same care we give new curricula.
- Equity at the center. Districts with fewer resources often struggle to enforce consistent rules or provide robust digital-literacy instruction. State and philanthropic support can ensure protective policies help close, not widen, existing gaps.
- Teach, don’t just police. Lessons on digital citizenship, emotional regulation, and online choices turn rules into real-world skills.
- Safety without constant connectivity. Classroom phones, teacher radios, and main office lines can make sure families can reach kids when needed — without every student holding a device all day.
- Make healthy tech habits part of the bigger picture. Cutting back phone use at school helps, but curbing risks like cyberbullying, social comparison, and compulsive use requires teamwork across schools, families, and communities.
A Balanced Path Forward
This isn’t about control. It’s about giving every student a learning environment where they can thrive. When districts, PTAs, and policymakers come together to craft smart, flexible guidelines — and commit to tracking what works — we can find the right balance between staying connected and staying focused.
The Child Mind Institute is ready to help states, districts, and school communities pilot, refine, and improve approaches grounded in evidence and shaped by experience. In schools that embrace thoughtful limits, students and teachers alike are reporting calmer days, better learning, and stronger real-world connections.
The research is clear. The mental health stakes are high. This is a challenge we can meet — and now is the time to act.
The post Phones Out, Focus In: Crafting Classroom Policies That Work for Everyone appeared first on Child Mind Institute.
]]>The post Understanding the Levels of Autism appeared first on Child Mind Institute.
]]>This is especially true since it is such a broad diagnosis that ranges from kids who are hyperverbal but socially awkward to those who are nonverbal and will require lifelong care. This is why the levels of autism were developed.
Previously, what is now known as autism spectrum disorder was four different diagnoses. Now there is one umbrella diagnosis with three levels of autism, which are based on the amount of support an individual requires in daily life.
Clinicians and autistic advocates have mixed feelings about the levels of autism. On the one hand, they can provide a helpful shorthand to give a sense of a person’s support needs. On the other, assigning a level is subjective and can oversimplify a complex condition.
Ultimately, it is often the families who crave the certainty of a level. “Parents are trying to figure out, if my child is on the autism spectrum, what does that mean for our family?” observes Alexis B. Bancroft, PhD, a psychologist at the Child Mind Institute Autism Center.
Ultimately, each child should be viewed as an individual with unique strengths and challenges. But the levels of autism can provide a general sense of the intensity of their needs.
What are the levels of autism?
The levels of autism were introduced in 2013, in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5). This was part of a consolidation of the autism diagnosis. What were previously four separate diagnoses — autistic disorder, Asperger syndrome, childhood disintegrative disorder, and pervasive developmental disorder-not otherwise specified — became one single diagnosis of ASD. They were combined because researchers argued that all the old diagnoses reflected the same underlying neurodevelopmental differences. The earlier diagnoses were overlapping and not consistently applied — two doctors might give different diagnoses to the same person. Once they were combined, the levels were added to indicate that individuals within the broad diagnosis have different degrees of impairment that call for different services.
“The reason they were created was because we wanted clinicians to be on the same page, and we wanted to differentiate between the levels of support that’s needed for each individual,” explains Dr. Bancroft. “But then there was no operationalized definition of what those categories mean.”
These levels are not based on intelligence or verbal ability, but on how much help someone generally needs to function in everyday life:
- Level 1 autism: requiring support
- Level 2 autism: requiring substantial support
- Level 3 autism: requiring very substantial support
Understanding these levels of autism can help parents, caregivers, and professionals create more effective, individualized care plans. But critics argue that the criteria for these categories are not standardized and are therefore subjective. Plus, the levels of autism can paint too broad a picture, leading people to make inaccurate assumptions about a person’s ability and cognition.
One receives a level of autism along with their autism diagnosis, regardless of age. And while an autistic person will always be autistic, their support needs — and therefore their level — may change as they mature and receive accommodations and services. One study found that 30 percent of autistic children had lower support needs at age six than they did at age three; it also can go the other way around as well, though that’s less common.
Children and adults at Level 1 may appear neurotypical in some settings but often struggle in specific situations. They may:
- Have difficulty initiating conversations or maintaining back-and-forth communication
- Misread social cues or facial expressions
- Prefer routines and resist change
- Show inflexible thinking patterns
These individuals — sometimes colloquially called “high functioning” — typically have strong verbal skills and average to above-average intelligence. However, they may have sensory sensitivities, social challenges, or have trouble with transitions. Still, they are often able to access mainstream educational settings with minimal support.
People diagnosed with Level 2 autism need more significant assistance in both social communication and daily living. Common traits include:
- Limited verbal and nonverbal communication skills
- Trouble coping with changes in routine or environment
- More noticeable repetitive behaviors (e.g., hand-flapping, rocking)
- Difficulty initiating or responding to social interaction, even with support
Individuals with level 2 autism may benefit from structured programs and therapeutic support that address both behavioral challenges and communication needs. But with accommodations like a 1:1 aide, they are often able to be placed in mainstream classrooms.
Level 3 autism represents the highest level of need and is sometimes referred to as profound autism. Children and adults at this level often have severe impairments in communication and behavior. They may:
- Be nonverbal or use very limited speech
- Display intense repetitive behaviors
- Struggle significantly with change or transitions
- Need assistance with self-care tasks like toileting or getting dressed
- Require 24/7 supervision or highly structured settings
This level of autism requires ongoing, intensive support, often involving a team of specialists such as behavioral therapists, occupational therapists, and special education professionals.
How clinicians use the levels of autism
While the levels of autism are included in the DSM-5, in practice it can be tricky for clinicians to apply them. “We will use the levels, but we don’t love the levels,” explains Dr. Bancroft. She says that because definitions have not been codified, assigning an autism level is subjective and can be inconsistent across practitioners.
Having an identified level can be a starting point for families who are beginning to understand where their child falls on this spectrum. But ultimately, it’s more complex than that.
When speaking with caregivers about an autism diagnosis, Dr. Bancroft prefers to discuss a matrix of support needs based on a range of circumstances. For example, an autistic child may have intense sensory sensitivities, high intellectual ability, occasional aggressive behavior, and difficulty communicating and interacting in some but not all situations. The levels of autism — in this case probably a Level 2 — would not capture this nuance but could act as a general summary.
“I do think the levels of autism provide something tangible and definitive for parents that could potentially be helpful if we were better at using them,” says Dr. Bancroft.
How schools use the levels of autism
The levels of autism can also be necessary in school settings and IEP meetings, where a level may be required to qualify for specific services. Educators may also benefit from a general sense of a student’s support needs. “One would assume that a child with Level 3 autism would require very substantial supports across all areas and more intensive intervention — meaning more services through an IEP — than a child with Level 1,” explains Dr. Bancroft. A child with Level 1 autism, meanwhile, could probably be placed in a general education setting with minimal related services.
Ultimately, understanding the different levels of autism can empower parents and caregivers to better advocate for their children. Recognizing early signs, seeking a professional autism diagnosis, and tailoring support to a child’s needs can make a lasting difference. The levels can be a helpful snapshot as long as we recognize the nuance of the individual experience. “I think we need to be careful to not assume a child’s ability or capability based off of the level of support that they need,” urges Dr. Bancroft. “We need to assume that they are capable, and we want to support them to become as independent and capable as they are able.”
The post Understanding the Levels of Autism appeared first on Child Mind Institute.
]]>The post How Young Children’s Play Promotes Healthy Development appeared first on Child Mind Institute.
]]>Imaginative and child-led play
Children begin engaging in different kinds of imaginative play around age 2. In the toddler years, many children start acting out familiar events in their play, like rocking a baby doll or putting pretend food on a plate. This kind of play becomes more complex and creative in the preschool years, at times involving imaginary objects and detailed storylines. Pretend play can support learning outcomes and skill development in vocabulary, creativity, emotion regulation, and short-term memory, among others.
Grown-ups can encourage play by joining in the fun! Caregivers can facilitate the natural learning that happens in open-ended play by playing along and following the child’s lead, without directing the play. In child-led play, children choose what they want to play with and how they want to play. Regular, enjoyable playtime together is a powerful way for caregivers to support happiness and emotional well-being in their young children. And the impact on well-being is not just on the child! Studies have shown that playing with your child can lead to reduced parenting stress.
Caregiver Tips:
- Just 5 minutes a day of playtime can strengthen the caregiver-child relationship, especially if the caregiver joins the child’s play world and follows the child’s lead.
- Caregivers can encourage pretend play by modeling how to use objects creatively and by acting out characters.
Playing with other children
Children’s play becomes more complex and social around age 3. Providing young children with opportunities to play with other kids is important for their development and learning. In the early preschool years, children begin to shift from parallel play to cooperative and social pretend play with their peers. This may look like two children working together on a puzzle or pretending to work at an ice cream shop.
In play with peers, children build social and emotional skills as they face scenarios that require them to work together, solve problems, and consider others’ perspectives. The positive feelings that children have as they play together can also promote friendships.
Caregiver Tips:
- Playing pretend with your child at home can help them practice and develop the skills required to engage in social pretend play with other kids, like cooperation, perspective-taking, and flexibility.
- Young children benefit from adult scaffolding when challenges arise during social play, especially for more advanced social skills like problem solving and perspective taking.
Outdoor play and physical activity
Playing outside helps support healthy physical, social, cognitive, and emotional development in young children. In the outdoors, kids learn and develop as they explore nature, move around more freely, and challenge themselves through riskier play. For instance, a child might wade in a pond and collect pebbles, roll down a hill, or climb up onto a boulder. Outdoor play also creates endless opportunities for children to be creative and collaborative. This might look like your child pretending a stick is a magic wand or gathering a group together for a game of tag.
Physical activity is particularly important for preschoolers and kindergarteners, since they are growing and developing so quickly. Unfortunately, many young children are not getting enough physical activity each day, and only about half of preschoolers in the United States go outside to play at least once a day with a parent. Healthy levels of physical activity are linked to improved heart health, lung function, bone strength, and other important aspects of physical development and fitness. In addition to a range of health benefits, participating in physical activity leads to gains in young children’s social, motor, and cognitive skills. As young children find enjoyment through physical activity and outdoor play, they also build a foundation for future healthy habits and pro-environmental behaviors.
Caregiver Tips:
- Three hours of daily physical activity is recommended by the U.S. Physical Activity Guidelines for children under 6 years old.
- Take a step back while supervising outdoor play! Research increasingly suggests that the benefits of age-appropriate risky play on children outweigh the potential costs. This may look like letting your child climb to the top of a play structure or run quickly down a hill. Importantly, a risk is different than a hazard — adults should intervene if a child is in danger of serious injury.
Structured activities and sports
Early childhood structured activities, like classes and sports, can help your young child learn and develop their interests in a playful way. Young children find enjoyment in music, for instance, by singing songs, playing simple instruments, and listening to music. In music classes, children are encouraged to create or move along with music, which supports motor coordination. Through structured visual art activities like drawing, painting, and sculpting, young children can explore colors, textures, and shapes while also building their fine-motor skills and creativity.
Sports are a great way for your child to get active while having fun. Participating in a sport allows young children to build skills and challenge themselves as they work to learn the rules, physical techniques, and importance of teamwork. In fact, preschool-aged children who play sports or participate in organized physical activities appear to have better emotional health, social skills, and self-regulation abilities!
Many children this age will have a hard time staying fully engaged in a sport and playing by the rules. For example, they may run the opposite direction, score on their own goal, or twirl around on the field. If your child is having fun, they are reaping the benefits of these joyful experiences, which contribute to their overall well-being. Plus, research suggests that the number one reason kids play sports is because they find it fun.
Caregiver Tips:
- Early childhood is a great time to help foster interests by allowing your child to explore a range of activities. Structured activities for this age group should be mostly focused on fun and exploration. It’s highly unlikely your kid will love every sport or activity they try. Follow their lead and keep trying until your child finds what is right for them.
- Early childhood sports can be a great way to build community and meet other caregivers. Recreational and community sports leagues are a great way to get into youth sports, since they are often lower-cost and lower pressure. You can even volunteer to coach, regardless of whether you have prior experience playing the sport! Your primary job is to make sure the kids are having fun.
Link between play and subjective well-being
Play supports the healthy development of preschoolers and kindergarteners, and it also allows children to experience the positive emotions that are essential for subjective well-being. Early childhood is a time when kids are primed for creative thinking and learning. In fact, it is theorized that the fun that comes from play leads young children to explore further, try new things, and think flexibly. As kids have fun playing pretend, exploring nature, running around, or creating art, they have the potential to build lasting resources, including those related to relationships, skills, and overall health. Subjective well-being, or happiness, in childhood is linked to higher levels of empathy, social competence, self-regulation, resilience, and academic achievement. Early childhood play is all about having fun, but the benefits of play on children’s learning and development extend well beyond that!
The post How Young Children’s Play Promotes Healthy Development appeared first on Child Mind Institute.
]]>The post California Students Recognized for Designing Digital Interventions in Support of Teen Mental Health and Wellness appeared first on Child Mind Institute.
]]>Sacramento, CA — As young people navigate the complexities of the digital age, a new wave of solutions is emerging — designed by youth, for youth. Today, the California Department of Health Care Services (DHCS) and the Child Mind Institute, with support from the Children and Youth Behavioral Health Initiative (CYBHI), proudly announced the winners of the first Single-Session Intervention (SSI) Challenge. This groundbreaking competition invited California high school, undergraduate, and graduate students to design brief, scalable digital interventions aimed at fostering healthier and more intentional technology use.
The SSI Challenge is part of a broader California effort to engage youth in co-developing mental health tools that reflect their lived experiences and meet the evolving needs of their peers. All interventions were developed using the Child Mind Institute’s software MindLogger, supported in part by CYBHI. The submissions, which showcased remarkable creativity, empathy, and insight, ranged from mindfulness and cognitive restructuring tools to interactive guides for media literacy and fostering genuine social connection.
“At the Child Mind Institute, we believe young people should be part of the solution when it comes to supporting their mental health,” said Dr. Harold S. Koplewicz, founding president and medical director of the Child Mind Institute. “These interventions show that when we give youth the tools and the trust, they can create meaningful, scalable solutions that meet their peers where they are — online.”
“California’s CYBHI is committed to keeping youth at the center to better meet them when and where they need it most,” said Dr. Sohil Sud, director of the CYBHI. “When we listen to young people and equip them to lead, we create more relevant and impactful behavioral health supports.”
The winning projects tackle a diverse array of topics vital for today’s youth, including emotional regulation, self-esteem, values-based decision-making, media literacy, and digital boundaries. The common thread? Each was designed with a profound understanding of the digital world from the perspective of those most immersed in it.
High School Winners
Stephanie Leung, Mission San Jose High School, Fremont, California — “Rethink Agency: Reclaiming and Redefining Tech Use”
A reflective three-step intervention that guides teens in rethinking the impact of tech on their well-being, reclaiming personal agency, and setting healthy boundaries.
Zenia Rehan, Castilleja School, Palo Alto, California — “Scroll Control”
Helps participants examine their social media habits and create personalized specific, measurable, achievable, relevant, and time-bound (SMART) goals, incorporating peer testimonials and data collection to improve agency.
Riyana Melvani, Monte Vista High School, Danville, California — “Mindfulness in the Digital World”
Guides participants through three self-paced activities to reflect on the content they consume, their digital self-presentation, and the impact of technology on their mental well-being, fostering a more intentional relationship with social media.
Undergraduate Winners
Selena Cuevas and Andrew Alvarez, University of California, Berkeley — “Overcoming Triggers From Social Media Using A.C.C.E.P.T.S.”
A Dialectical Behavior Therapy (DBT)-informed intervention that provides youth with tools to regulate emotional distress from social media through grounding, reframing, and resilience-building techniques.
Diana Vega, University of California, Irvine — “Cognitive Restructuring”
Teaches users how to recognize and reframe negative self-thoughts, particularly those triggered by comparison online, using relatable storytelling.
Sarah Arcelo, University of California, Berkeley — “Mind Over Media”
Uses mindfulness to help teens reflect on emotional triggers for screen use and develop healthier, more intentional tech habits.
Graduate Winners
Iris Khan, California State University, San Bernardino — “Overcoming Social Barriers: Rethinking Tech Use”
Focuses on building psychological capital to help youth set social goals and leverage technology to form more meaningful relationships.
Madhuri Sharma, Elizabeth Garcia, and Srinidhi Vusirikala, Santa Clara University — “Beyond the Filter”
A media literacy and GenAI intervention helping teens, especially girls, build confidence in navigating digital spaces and understand how AI alters body image online.
Ellie Xu, University of Southern California — “Valued Living With Healthier Technology Use”
Based in Acceptance and Commitment Therapy, this intervention helps youth define their values and align their digital habits with those values through committed action.
What Comes Next?
These pioneering interventions will undergo further validation and refinement. The goal is to make these youth-developed tools accessible to young people across California.
Learn more about the SSI Challenge.
Media Availability
Interviews with representatives from the Child Mind Institute, CYBHI, and select student winners can be arranged. Visual assets, including logos and screenshots of the MindLogger platform, are available upon request.
About the Child Mind Institute
The Child Mind Institute is dedicated to transforming the lives of children and families struggling with mental health and learning disorders by giving them the help they need. We’ve become the leading independent nonprofit in children’s mental health by providing gold-standard evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing tomorrow’s breakthrough treatments.
About the Children and Youth Behavioral Health Initiative (CYBHI)
The CYBHI, led by the California Health and Human Services Agency and DHCS, is reimagining and transforming the way California supports children, youth, and families. CYBHI is investing in a coordinated ecosystem of services that prioritize prevention, early intervention, and youth-driven design. By centering the needs of young people and uniting the efforts of the agencies and organizations that serve them, the CYBHI seeks to ensure kids and families can find support for their emotional, mental, and behavioral health needs, when, where, and in the way they need it most.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post California Students Recognized for Designing Digital Interventions in Support of Teen Mental Health and Wellness appeared first on Child Mind Institute.
]]>The post California Students Take the Lead on Tech and Mental Health appeared first on Child Mind Institute.
]]>The Child Mind Institute is thrilled to announce the winners of the inaugural 10-Minute Challenge, a statewide competition that invited California students to take the lead in designing digital solutions that support healthier technology use and youth mental health.
Co-hosted by the Child Mind Institute and the state of California’s Children and Youth Behavioral Health Initiative (CYBHI), this first-of-its-kind challenge called on high school, undergraduate, and graduate students to create brief, research-informed digital tools — called single-session interventions (SSIs) — that help young people better understand and manage their relationship with technology.
Leveraging the Child Mind Institute’s open-source platform MindLogger, the winning interventions showcase an inspiring combination of lived experience, empathy, and scientific creativity. From mindfulness practices to media literacy and values-based reflection, these submissions demonstrate what’s possible when we empower young people to design solutions for their peers.
Our winning submissions, found below, are those that our interdisciplinary team of judges found most intriguing, and worthy of moving into the next phase of research validation.
"These interventions show that when we give youth the tools and the trust, they can create meaningful, scalable solutions that meet their peers where they are — online."Dr. Harold S. Koplewicz, President and Medical Director, Child Mind Institute
High School Winners
Stephanie Leung, Mission San Jose High School
A reflective three-step intervention that guides teens in rethinking the impact of tech on their well-being, reclaiming personal agency, and setting healthy boundaries. The goal of this intervention isn’t to shame tech use, but to empower you to use tech in a way that supports your well-being, instead of working against it.
Zenia Rehan, Castilleja School
Helps participants examine their social media habits and create personalized SMART goals, incorporating peer testimonials and data collection to improve agency.
Riyana Melvani, Monte Vista High School
Guides participants through three self-paced activities to reflect on the content they consume, their digital self-presentation, and the impact of technology on their mental well-being, fostering a more intentional relationship with social media.
Undergraduate Winners
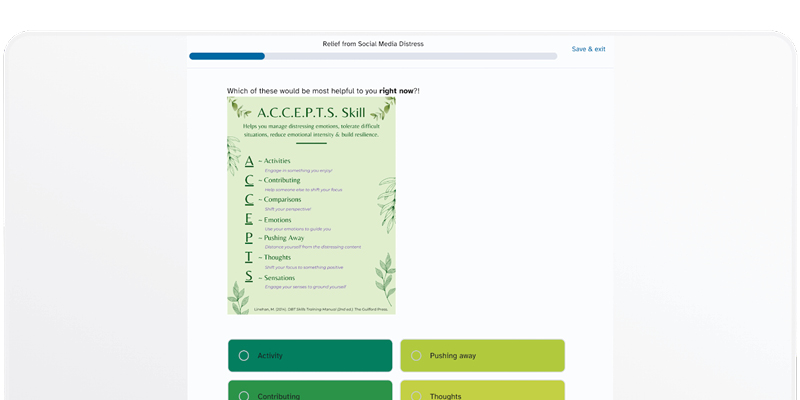
Selena Cuevas and Andrew Alvarez, UC Berkeley
A DBT-informed intervention that provides youth with tools to regulate emotional distress from social media through grounding, reframing, and resilience-building techniques. It seeks to give young people specific tools to handle emotional distress from social media, using strategies like grounding techniques, cognitive reframing, and resilience-building.
Diana Vega, UC Irvine
Teaches users how to recognize and reframe negative self-thoughts, particularly those triggered by comparison online, using relatable storytelling.
Sarah Arcelo, UC Berkeley
Uses mindfulness to help teens reflect on emotional triggers for screen use and develop healthier, more intentional tech habits.
Graduate Winners
Iris Khan, CSU San Bernardino
This intervention focuses on building psychological capital, guiding participants towards recognizing how social media can be a tool for avoidance behavior, and then reframing it as a resource that can help build meaningful social relationships.
Madhuri Sharma, Elizabeth Garci, and Srinidhi Vusirikala, Santa Clara University
A media literacy and GenAI intervention helping teens, especially girls, understand how AI alters body image online and build confidence in navigating digital spaces.
Ellie Xu, USC
Based in Acceptance and Commitment Therapy, this intervention helps youth define their values and align their digital habits with those values through committed action.
What’s Next?
These winning entries will now move to the next phase of development and research, with the potential to be scaled across California as evidence-based mental health tools for young people. Select teams will have the opportunity to present their work at the International Single Session Therapies Symposium (SST5) and potentially co-author research with Child Mind Institute scientists.
Visit the 10-Minute Challenge event page to explore these winning entries and learn how the Child Mind Institute and the Children and Youth Behavioral Health Initiative are empowering the next generation of mental health advocates. We extend our heartfelt congratulations to all participants. Your voices, ideas, and leadership are shaping the future of youth mental health — and we can’t wait to see what you build next.
The post California Students Take the Lead on Tech and Mental Health appeared first on Child Mind Institute.
]]>The post Why Are Black Parents Concerned About Medication Treatment? appeared first on Child Mind Institute.
]]>This sentiment — expressed by a participant in a recent study that explores the views and experiences of Black families and young adults seeking mental health care — reflects a common concern within the Black community.
The study, conducted by the Child Mind Institute in partnership with The Steve Fund, included a nationally representative survey of 1,000 Black parents seeking mental health care for their children and 500 young adults seeking care for themselves. When asked about their concerns around mental health care, about half of the respondents (both parents and young adults) agreed that “mental health professionals are too quick to prescribe medication for mental health issues.”
This sense of mistrust around medication treatment is also reflected in other studies. For instance, a 2021 review of data on African American caregivers deciding whether or not to give children with ADHD medication, caregivers were less likely to trust the efficacy of the medication and were more concerned about side effects and addiction than white caregivers.
“I work in an integrated mental health system, which includes psychiatry. So, concerns about medication come up a lot,” says Rhonda Boyd, PhD, a mental health advisor for The Steve Fund, psychologist, and associate director of the Children’s Hospital of Philadelphia’s (CHOP) Child and Adolescent Mood Program. “Black families in particular want to start with therapy first and see how it works before considering medication if therapy is not working.”
One source of medication reluctance, Dr. Boyd says, is concern about side effects — will it stunt their child’s growth? But it also may come from feeling pressure from schools. “Schools oftentimes refer kids for treatment if the kid’s behavior is disruptive, which could be for a number of reasons. And that’s where the pressure comes in — you have to do this, or we can’t treat your child in a regular classroom. They may not even be able to be in this school.”
But concerns about medication run deeper, in no small part because of the historical use of psychiatric medication to silence and control Black people in the United States.
The history of overmedicating Black patients
Historically, the overmedication of Black patients in the mental health care system has been linked to their frequent misdiagnosis. The background of schizophrenia characterization and diagnosis is a clear example.
In the late 1950’s, as psychiatric hospital wards began to desegregate and the Civil Rights Movement gained momentum, the second edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-II) was published. Schizophrenia previously had been separated into subtypes, including “paranoid schizophrenia,” which was characterized by delusions and/or frequent auditory hallucinations. But in the DSM-II, researchers redefined characteristics of that subtype as a “masculinized belligerence” in which patients displayed violent delusions, hostility, and aggression. Based on racial bias, researchers and clinicians began to associate this type of schizophrenia with Black patients — specifically Black men. Schizophrenia diagnoses among Black individuals drastically increased, and by 1969, the National Institute of Mental Health found that Black patients had “a 65% higher rate of schizophrenia” than white patients.
As more Black people were diagnosed with schizophrenia, psychiatrists started to conflate civil unrest with the disorder’s “violent delusions” characteristic. Two prominent New York psychiatrists coined the term, “protest psychosis,” arguing that Black Liberation rhetoric and art caused hallucinations and acts of violence among Black men. In response, clinicians argued Black patients should be given higher doses of tranquilizing antipsychotic medication to quell these violent tendencies. For Black patients, medication transitioned from treatment to a form of control.
While the language in the DSM has since changed, recent studies have shown that Black Americans are still 2.4 times more likely to be diagnosed with schizophrenia than their white counterparts. Additionally, researchers have found that Black patients are more likely to receive higher doses of long-acting antipsychotic drugs — indicating a persistent belief among providers that Black patients not only need more medication than typically necessary but are also less likely to take it as prescribed.
How are Black children directly impacted?
This idea that Black people are inherently more prone to violence and disruption continues to be perpetuated to this day. And in classrooms, Black children are much more likely to be viewed as disruptive or displaying behavioral challenges than their white counterparts.
“If Black and brown children display behavioral challenges like biting or hitting — things that you may see in the pre-K years or early childhood years where this type of behavior is developmentally appropriate — these children are seen as more aggressive, more forceful, and much more of a concern,” explains Robert Harris, an early childhood intervention supervisor for the D.C. Healthy Futures Program.
Worried about the disruption in learning, educators are quick to find a solution — and this most likely involves referring the child to a mental health professional. But according to Harris, “Even in the referral process and the description of the challenge, they tend to lean towards or hint at the use of medication to mitigate this issue that may exist. This is before parents have even spoken to a mental health professional.”
So, by the time parents are consulting a provider, they may already have their guard up, especially if that provider goes on to prescribe medication for their child’s mental health issues.
How can clinicians work with skeptical parents?
Clinicians worry that in some cases, reluctance towards medication treatment runs the risk of impeding a child’s quality of life. “Negative perceptions about medication can delay treatment longer than you want,” says Dr. Boyd. “If someone has severe depression, for instance, what is recommended is both therapy and medication at the same time to get the kid out of that episode. I understand exactly why parents have concerns, but it can be frustrating.”
To find the best solution for the child’s mental health challenges, the first critical step is to create a comfortable and collaborative environment, according to Jonathan Shepherd, MD, a child, adolescent, and adult psychiatrist who is chief clinical officer at DC Department of Behavioral Health. “For those initial appointments, I do my best to develop a form of trust where they feel comfortable enough with me,” he says.
And to do so, Dr. Shepherd suggests the following:
- Educate yourself. Dr. Shepherd points out that when a mental health professional isn’t Black, it’s hard for Black patients to feel like the provider will understand where they’re coming from. Given the history of mistreatment of Black patients, there’s a hesitancy to even reach out to a provider. “You have to understand what that person may be going through or what environment they live in. It’s very difficult for people who don’t understand Black culture to be able to say, ‘I understand what it took for you to even come see the doctor.’” So, it’s important for non-Black providers, especially, to take that extra step and educate themselves on the history of mental health in the Black community.
- Listen to their concerns and answer every question. When encountering parents who are wary of treating their child with medication, Dr. Shepherd starts the conversation by saying, “You have every right to be skeptical and hesitant regarding care for your children. I get it. It is scary to think about providing a medication for your child, or your child having to take a pill and you don’t know what that pill may do. But that’s where the experts come in. Now, what I will not do is force my help on you, but I will work alongside you to guide you through the process.
- Be patient and meet them where they’re at. Dr. Shepherd acknowledges that after he explains why he’s prescribing the medication, describes the side effects, and answers every question, he still might face some resistance from a parent — and that’s okay. Instead of pushing, he schedules a follow-up appointment to continue the conversation at a different time. He also provides them with some helpful resources to gain more information about different treatment options. “You have to be very careful about the websites that people are going to, to seek out information. So, steer them in the right direction.”
How can parents advocate for their child?
When a school is pushing for a quick solution to a child’s disruptive behavior, such as medication treatment, parents may feel backed into a corner. Harris wants them to know that there’s still a choice. And if you feel uncomfortable with what you’re being told, you can say, “Yeah, when you said this, it really made me feel like I needed to go for medication.” This way, says Harris, educators might take a step back and re-evaluate how they approach the situation.
He also reiterates the importance of parents arming themselves with the knowledge of early signs to look for in their child, whether it’s a behavioral issue, mental health disorder, or learning challenge. “I think that’s why mental health consultation, particularly for infant and early childhood is paramount, because through education, we provide families as well as professionals with an understanding of what’s appropriate, what’s typical, what’s developmentally acceptable, and what you should expect.” For instance, it can be helpful for parents to know that there are several alternatives to medication treatment for disruptive behavior in a classroom, such as therapy, parent training, specialized programs, and a change in classroom structure.
And in a clinical setting, Dr. Shepherd says, if you’re feeling skeptical about what your provider has prescribed for your child, you can start by making it clear to them that you don’t feel like they’re hearing you. “You can say, ‘I’m not sure if we’re hearing one another. I’m not sure that we are on the same page regarding what I’m saying I see in my child or what I think is necessary for my child at this point in time.’”
And that’s when it’s important to pay attention to the provider’s reaction, says Dr. Shepherd. Are they receptive to what you have to say? Are they open to answering questions or engaging in a dialogue about different treatment options? “Someone who does not allow you to ask questions or glosses over your questions, that’s a physician that you should run from.”
When parents and providers are able to have the tools and language they need to enter these types of conversations, it can make finding the solution to a child’s mental health challenges much easier.
The post Why Are Black Parents Concerned About Medication Treatment? appeared first on Child Mind Institute.
]]>The post Introducing You Are Okay: A New Mental Health Resource for Young People appeared first on Child Mind Institute.
]]>At the Child Mind Institute, we believe that every young person deserves straightforward guidance they can trust. That’s why we’re excited to announce the launch of You Are Okay, a new digital resource created specifically for teens and young adults navigating mental health challenges.
What Is You Are Okay?
You Are Okay is a resource hub designed to give young people the tools, knowledge, and support they need to care for their mental health. Guided by the same values as the Child Mind Institute’s Family Resource Center, You Are Okay offers content that’s expert-backed, easy to understand, and actually speaks to what it’s like to grow up right now.
What You’ll Find
- Mental health guides written for teens and young adults, covering topics like anxiety, depression, self-harm, relationships, and more.
- A growing community where young people can share their stories and experiences — because knowing you’re not alone is powerful.
- Content that’s helpful, hopeful, and honest — always.
Find You Are Okay On:
- Instagram — @YouAreOkay
- TikTok — @youareokayHQ
- YouTube — @youareokayHQ
A Personal Connection
You Are Okay began as the passion project of Jenny Jaffe, an Emmy-nominated comedy writer and performer, who grew up with mental health challenges and wanted to make it easier for others to get help, talk about how they’re feeling, and find their way forward. Her vision of empathy, creativity, and courage lives at the heart of everything we do.
Whether you’re a young person, a parent, an educator, or just someone who cares, we hope you’ll explore youareokay.org. And if you know someone who could use it, please pass it on. Sometimes, knowing there’s a place built just for you can be the first step toward feeling better.
The post Introducing You Are Okay: A New Mental Health Resource for Young People appeared first on Child Mind Institute.
]]>The post Mental Health Is Biological: Why Is That So Hard to Accept? appeared first on Child Mind Institute.
]]>By Michael P. Milham, MD, PhD
Chief Science Officer, Child Mind Institute
We hear it all the time: Are we “medicalizing” normal variations in human behavior? Is ADHD just a misapplied label for restlessness? Is clinical anxiety merely excessive worry — or does it reflect genuine differences in how the brain processes stress? Although ADHD often prompts these debates, similar questions swirl around autism, depression, PTSD, and other brain-based conditions. Headlines flip from “breakthrough biomarker found” one day to “biological links debunked” the next, leaving families, educators, and clinicians exasperated.
For neuroscientists and mental-health professionals, it is not controversial that ADHD, autism, depression, PTSD, and related conditions have neurobiological roots. Decades of genetics, neurochemistry, and brain-imaging research confirm that neural circuitry and chemistry matter. The tricky part is that patterns are clear when we look at large groups, but much harder to spot in one person.
At the group level — when data from hundreds or thousands of people are analyzed — we detect reliable patterns confirming disruptions in brain function, suggesting that a brain pathway may run faster or slower, or that a cortical region is fractionally thinner. At the individual level, however, those same differences are often obscured by natural variation from one person’s brain to the next. It’s like knowing Steph Curry averages 24 points per game — you can detect a reliable pattern across many games—but it won’t tell you if he scored 10 or 50 on a particular night. Group-level brain findings work the same way: they show real, measurable effects, but they may not always be useful for pinpointing what’s going on in a single person at one point in time.
Consider asthma and air-quality research: we know airway inflammation underlies the condition, yet pollution, allergens, and stress govern who develops symptoms and when. There are no obvious lesions on a scan, and no single region lights up to explain everything. Mental health disorders are similar. We must hunt for multiple, subtle signatures — an endeavor that demands patience, sophisticated tools, large datasets, and replications. Fortunately, advances in high-resolution brain imaging, digital monitoring, machine-learning algorithms, and artificial intelligence are accelerating our ability to spot these subtle patterns. This is the modern face of the long-running “nature-versus-nurture” debate: biology provides the wiring, but experience fine-tunes how — and whether — those circuits spark when challenged.
Three key concepts from developmental science illustrate how biology and environment shape mental health across childhood and adolescence. This ongoing interaction between biology and experience is best understood through three complementary frameworks that scientists regard as cornerstones of developmental health — how brains and behaviors evolve from infancy through adulthood.
Differential susceptibility — sometimes called the “orchid-and-dandelion” model — shows that children differ in biological sensitivity to their surroundings. “Orchids” thrive spectacularly in nurturing conditions but can wither under stress; “dandelions” are less reactive, doing reasonably well in almost any soil.
Building on that idea of uneven sensitivity, the two-hit hypothesis explains how timing matters: a first “hit” (such as a genetic vulnerability or perinatal complication) may sit silently for years until a second “hit” (e.g., puberty, a head injury, sustained bullying) pushes the system past its tipping point and visible symptoms emerge.
Finally, stress-inoculation theory offers a hopeful counterbalance. It shows that brief, manageable challenges — speaking in front of a class, tackling a difficult project with support — can act like a training vaccine, fortifying the brain’s coping circuits for future adversity.
Together, these models clarify why the same life event can derail one child, barely register for another, and actually strengthen a third: Biology sets the reactivity dial, environment turns the knob, and timing shapes the final outcome.
The clinical categories outlined in the official Diagnostic and Statistical Manual — even though they often arise from meticulous bedside observation — do not map neatly onto separate neural circuits. As Tom Insel, former director of the National Institute of Mental Health, observed, “the brain didn’t read the DSM.” History shows that astute clinical clues can unlock biology: think of how Rett syndrome, Fragile X, or specific heart-rhythm patterns pointed researchers to the underlying genes and pathways. The challenge for psychiatry is similar, but the signals are subtler and more distributed. Moving from broad labels, like “ADHD” or “depression,” to precise brain-based subtypes will require not just patience but also innovation — richer, smarter, and more individualized brain imaging; real-time digital phenotyping; advanced analytics; and cross-disciplinary methods that can capture the brain’s complexity on an individual level.
Recognizing a brain basis for mental health disorders doesn’t erase the role of the environment. Brains are shaped by both genetics and life experience — by trauma and chronic stress, but also by stable communities, good nutrition, and supportive relationships. Biology and context continually interact, influencing not just whether someone develops symptoms, but how they cope, recover, or even grow.
What this means for families
- Conditions like ADHD, depression, and autism reflect real brain-based differences, and even subtle signs deserve attention.
- No single blood test or scan can diagnose these conditions today, but precision psychiatry is rapidly coming into focus.
- Continued research will clarify biomarkers and counter claims that we are “over-medicalizing” human behavior.
Sensational headlines that frame mental health as “over-medicalization” only serve to fuel confusion and stigma. Every stable difference in behavior rests on a biological substrate — even if that substrate is subtle and hard to detect in a single person.
When we say “Why Is That So Hard to Accept?” we’re issuing a wake-up call. Let’s anchor our understanding in the undeniable — if nuanced — reality that mental health and its disorders reside in the brain. Admitting complexity is not denying reality. With continued research and ever-improving tools, we can advance toward truly personalized, compassionate mental health care — free from buzzwords and grounded in biological truth.
The post Mental Health Is Biological: Why Is That So Hard to Accept? appeared first on Child Mind Institute.
]]>The post The Stavros Niarchos Foundation (SNF) Global Center in Partnership with Radio Workshop Announces Next Generation of African Media Leaders Through Innovative Communicator Fellowship appeared first on Child Mind Institute.
]]>New York, NY, USA and Johannesburg, South Africa — The Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute is proud to announce the first cohort of Communicator Fellows from South Africa, delivered in partnership with Radio Workshop, a leading youth media organization that trains young people across Africa in radio and podcast production, with up to nine million monthly listeners. This inaugural Radio Workshop cohort builds on the program’s early success, following an initial fellowship awarded in partnership with the Carter Center.
The fellowship is part of a broader initiative of the SNF Global Center for Child and Adolescent Mental Health to support emerging communicators in underserved communities who are using media to fill a critical gap in promoting mental health, reduce stigma, and drive evidence-informed dialogue.
During their collaboration, SNF Global Center Communicator Fellows will produce a series of podcast episodes on child and adolescent mental health in South Africa. Over their two-year fellowship, senior fellows Mary-Ann Nobele and Naomi Grewan will mentor four junior fellows, this year they will mentor Curtis Mkhize and Sikelela Rollom. Through personal storytelling, on-the-ground reporting, and youth-centered perspectives, the fellows will lead the charge in transforming mental health conversations, combating misconceptions, and bringing critical attention to challenges facing young people today.
“Today’s mental health landscape requires bold new voices that move away from traditional narratives by blending unique insight and cultural understanding to drive real impact. That’s why we are excited to partner with Radio Workshop in supporting the first cohort of Communicator Fellows who have demonstrated how they can create powerful new narratives through professional skills and lived experiences,” said Peter Raucci, Director of the SNF Global Center Fellowships Program.
For 18 years, Radio Workshop has trained young people across Africa to use radio and podcasts to tackle the issues that matter to them. One topic that often comes up is mental health because it’s key to their well-being and their ability to help their communities.
“We are grateful for the partnership because it offers us an opportunity to help raise awareness, improve access to care, and be a part of the amplification of youth voices in the mental health conversation,” said Vuyo Lutseke, executive director of Radio Workshop.
Drawing from their exceptional experience and knowledge, the fellows share a connected determination to dismantling barriers towards quality mental health care for young people through compelling stories.
Curtis Mkhize, based in Durban, was first introduced to Radio Workshop in 2019 as a youth reporter at Vibe FM. His early experiences sparked a deep commitment to community work and youth empowerment. Today, Curtis uses storytelling to foster connection, raise awareness around mental health, and inspire collective action.
“Serving as a fellow is an exciting opportunity to grow as a leader and contribute to positive change,” said Mkhize.
With a similar passion for being a vocal advocate in her community, Sikelela Rollom began her journey in radio at Nkqubela FM, where she hosted youth programs exploring mental health, sexual and reproductive health, and climate change. She now works as a news reporter, radio presenter, and executive news producer at Nelson Mandela University’s Madibaz Radio, and has contributed to public health campaigns with Vuselela Media and UNICEF.
“I’m passionate about storytelling that makes a difference in my community,” she said. “This fellowship is a chance to build on that work.”
Mary-Ann Nobele is a radio journalist, youth advocate, and creative storyteller whose work has focused on education, mental health, and amplifying youth voices. With a background in podcasting and award-winning projects, Mary-Ann is passionate about using the fellowship opportunity to continue to drive meaningful conversations that resonate with young audiences through media.
Naomi Grewan is an audio documentary producer based in Johannesburg who has reported on social justice issues including lead exposure in Zambia and LGBTQI+ rights across Africa. A graduate of Rhodes University’s journalism program, Naomi brings a deep belief in storytelling for social change and a commitment to uplifting underrepresented voices.
Fellows receive an unparalleled opportunity for mentorship, production support, capacity-building and funding to develop content that centers the mental health needs and experiences of youth in their communities and promotes sustainable change. Fellows will create original podcast episodes exploring child and adolescent mental health, to be broadcast on local South African radio stations and shared via Radio Workshop’s website and streaming platforms like Spotify, Apple Podcasts, and Stitcher.
Together, the SNF Global Center and Radio Workshop are cultivating the next generation of South African media leaders—empowering them to tell bold, honest, and impactful stories that advance child and adolescent mental health.
To learn more about the Communicator Fellowships and the SNF Global Center, visit childmind.org/global.
To listen to episodes of the Radio Workshop podcast, visit radioworkshop.org.
This work is conducted by the Stavros Niarchos Foundation (SNF) Global Center at the Child Mind Institute with founding support from the Stavros Niarchos Foundation (SNF) as part of its Global Health Initiative (GHI).
About the SNF Global Center at the Child Mind Institute
The SNF Global Center brings together the Child Mind Institute’s expertise as a leading independent nonprofit in children’s mental health and the Stavros Niarchos Foundation’s (SNF) deep commitment to supporting collaborative projects to improve access to quality health care worldwide. The center is building partnerships to drive advances in under-researched areas of children’s and adolescents’ mental health and expand access to culturally appropriate trainings, resources, and treatment in low- and middle-income countries. This work is conducted by the Child Mind Institute with support from SNF through its Global Health Initiative (GHI).
About the Child Mind Institute
We are the leading independent nonprofit in children’s mental health providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing open science initiatives and tomorrow’s breakthrough treatments.
About Radio Workshop
Founded in 2006 as the Children’s Radio Foundation, Radio Workshop has trained over 5,000 youth reporters at more than 100 radio stations in 10 African countries, reaching up to 9 million listeners weekly. Through training programs and an acclaimed podcast series, Radio Workshop equips young people with the tools and skills to produce creative, community-rooted, and fact-based audio journalism.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post The Stavros Niarchos Foundation (SNF) Global Center in Partnership with Radio Workshop Announces Next Generation of African Media Leaders Through Innovative Communicator Fellowship appeared first on Child Mind Institute.
]]>The post Meeting the Mental Health Needs of Black Adolescent Boys appeared first on Child Mind Institute.
]]>When Brandon Jones was a public school counselor in Minneapolis, he heard those words regularly from a 12-year-old Black male student who wore a tough exterior amid a dysfunctional home life. But after three or four months of therapy sessions, Jones says, the young man stopped mentioning it.
“I remember I asked him, ‘Why are you still coming here? Because your grandma wants you to come here?’ He was like, ‘No, I come here because I like you,’” says Jones, who wears jeans and Jordan sneakers just like his young clients do.
Now the executive director of the Minnesota Association for Children’s Mental Health, Jones crossed paths with the student over a decade later. The former counselor sees how being “a voice of reason” and helping the student “see a future for himself” may have had a positive effect on him. A life that could have ended in incarceration or premature death transformed into one of service instead, as the student had become a basketball coach in the same school district where they’d met.
“I would just try to say, ‘Man, you have so much talent. You’re so smart. You don’t have to do these things,’” Jones recalls.
Despite having an overall positive attitude toward mental health care, many young Black males are resistant to professional care, according to the Mental Health Support for Black Families study conducted by the Child Mind Institute in partnership with The Steve Fund. The study — which surveyed 1,000 Black parents seeking mental health care for their children and 500 Black young adults seeking care for themselves — found that young male participants were less likely than their female counterparts to seek help from a mental health professional. Among survey participants, 44 percent of young Black males (compared to 31 percent of females) said they were more likely to turn to family members and friends for support, with 37 percent (compared to 24 percent of females) seeking out church leaders.
Barriers to care for young Black men
Results of the survey suggest that the hesitation of young Black males to seek professional mental health care could be due to stigma. While both parents and young people said they were concerned about stigma, young adults were more likely than parents to say that stigma prevented them from seeking care.
And lack of trust in mental health professionals may be a legacy that historians can trace back to slavery. In 1848, John Galt, the medical director of the Eastern Lunatic Asylum in Williamsburg, Virginia, said that “Blacks are immune to mental illness.” He also stated that enslaved Africans were “exempt” from mental illness because they didn’t own property, and that people who had the highest risk of psychiatric illness were those who were exposed to the “mental excitement” of a free life.
In spite of this false ideology, in 1868 the Freedmen’s Bureau negotiated with the Virginia legislature to open the Central Lunatic Asylum for Colored Insane — the first mental asylum for Black Americans. This was an important step towards acknowledging the mental health needs of Black people. But historians have noted that medical racism and implicit bias among clinicians contributed to high rates of admission and severe diagnoses.
In the late 1950s, when psychological hospitals began to desegregate and the Civil Rights Movement gained momentum in the United States, clinicians would use a schizophrenia diagnosis to categorize Black men as violent and unstable. They especially applied this label to those who spoke out against racial injustice. The rates of schizophrenia diagnoses remain disproportionately high among Black men to this day.
“Some studies have revealed that Black men see professional mental health-seeking as a sign of weakness,” says Annelle Primm, PhD, a licensed psychiatrist and senior medical director at The Steve Fund. “And with high rates of misdiagnosis of schizophrenia among Black males and involuntary inpatient hospitalization, help-seeking through informal sources may be seen by Black males as a safer alternative.”
The dangers of bias and misdiagnosis
Unfortunately, even after Black males overcome stigma and make it to a mental health professional’s office, more barriers exist. There, they may be met with continued bias.
“When a person sees a Black man who’s emotional, they see us as an angry being. They don’t see us as a person who may actually have a disorder,” says Jonathan Shepherd, MD, a psychiatrist and chief clinical officer at the D.C. Department of Behavioral Health.
A costly consequence of racial bias in a mental health setting is misdiagnosis, especially of mood disorders.
“You have to be with a skilled mental health professional who can tease out the difference between ADHD and a mood disorder, because some of the symptoms overlap,” Dr. Shepherd says. “A person who has depression has poor concentration.”
Research shows that Black kids are more likely to receive the wrong diagnosis when they show signs of a mood disorder. For example, a Black boy who is inattentive or fidgety in class may be diagnosed with ADHD or a conduct disorder, while his white classmate with the same symptoms may be diagnosed with depression.
“How you treat ADHD and how you treat depression are two totally different ways,” Dr. Shepherd says about the dangers of receiving improper treatment.
Additionally, reactions to trauma and adverse childhood experiences — such as living in a hostile neighborhood or having an incarcerated loved one — share the same symptoms of ADHD: agitation, restlessness, and volatility. Without the correct diagnosis, Black males don’t receive the proper care and risk remaining stuck in unhealthy cycles.
For this reason, it comes as no surprise to Dr. Shepherd that young Black males are leaning on loved ones, mentors, and church leaders for support.
“It makes perfect sense. Men need to have safe, confidential, and peaceful areas to express themselves.”
Why young Black males turn to church leaders for support
As a significant percentage of young Black males in the Mental Health Support for Black Families study said they were more likely to reach out to a church leader than a mental health professional for support, experts suggested that it would be beneficial to work with churches to encourage these young men to seek mental health care.
Pastoral counseling is an important part of the faith experience. In a study that included interviews from nearly 100 Black pastors, the respondents averaged more than six hours of counseling work per week, in which they often addressed serious problems similar to those seen by mental health professionals.
Keith Pettus, PhD, serves as lead pastor at Truth Center on Long Island, outside New York City. In the four decades that he’s worked as a minister, he’s counseled many Black boys and men navigating life’s issues.
“Pastoring gives you a front row seat to the darkest moments of people’s lives and the brightest ones,” Dr. Pettus reflects. “We are with people from the cradle to the grave.”
He agrees that one of the main reasons why Black males avoid mental health providers is due to a general distrust in medical professionals.
“The challenge with Black boys is they become Black young men, and they become Black adult men who don’t go to doctors,” says Dr. Pettus, who encouraged the men in his congregation to get check-ups after he survived prostate cancer last year.
Because therapists may be viewed as just “another doctor,” he believes it’s easier for his congregants to seek him out for support. Two of the main reasons why young Black males come to him is for low self-esteem and anxiety about the future.
How mental health providers can work with the church
As a former school counselor, Jones appreciates when faith leaders are involved in resolving the mental health needs of community members. He hopes to see more innovation and collaboration between the two groups in the future.
“It’d be amazing if there were therapists that were housed inside churches,” he suggests. “A lot of church buildings are not active after Sunday…. They could be mental health centers at this point. Or they could have therapists in there working.”
Historically, the church has functioned as a social service hub for Black Americans, providing information and resources that might otherwise be inaccessible. Church members also use it as an emotional outlet. With that in mind, researchers and organizations are utilizing the institutions to find new ways to address mental health needs.
In 2019, the University of Pittsburgh’s School of Social Work launched CHURCH (Congregations as Healers Uniting to Restore Community Health), a research initiative that seeks to develop evidence-based training to build more capacity for African American faith leaders to provide mental health support to their congregation members.
For the past four years Deborah Moon, PhD, a mental health therapist and assistant professor in the School of Social Work at the University of Pittsburgh and the CHURCH project team, has worked alongside local Black pastors to develop a training that would equip local Black pastors with the knowledge and skills in cognitive behavioral therapy (CBT), a form of talk therapy that helps people change negative thought patterns and behaviors.
“There’s lots of evidence that CBT works,” Dr. Moon says. “But then [in CHURCH], we try to highlight that those same principles that are proven by science are already in the Bible.”
She and her team compiled a day-long workshop as the final curriculum. The program was separated into four sessions that covered the relevance of mental health topics in Black churches and the various levels of human cognition that are targeted in CBT. All sessions integrated core CBT principles and skills with spiritual teachings in Black churches. The workshop also included a music therapy element within the faith-based praise and worship. Their main goals were to change attitudes toward evidence-based mental health treatment, raise confidence in providing informal mental health support, and increase the knowledge of CBT concepts and skills among faith leaders in culturally sensitive ways through spiritual integration.
“We saw significant improvement in all of those areas in a recent pilot,” Dr. Moon says. The team is planning to conduct larger studies with a sufficient number of participants to more rigorously test the training effects. Like the participants of CHURCH, Jones recommends that all pastors who respond to mental health needs take up some form of CBT education. Dr. Pettus, the pastor at Truth Center, agrees but also sees the limits of what spiritual advisors can do. If he feels that a matter requires clinical services, he refers congregation members to therapists in the area.
“I’m not the last step. I have people above me that can take them even deeper.”
How can parents and mentors provide support?
Jones offers the following tips to parents and mentors who seek to support young Black males:
Parents:
- Keep an open space for your child to talk to you. If your children are coming to you, that’s a big plus. A lot of times when kids are avoiding talking to their parents, Jones has found, it’s because the parents are part of the problem
- Model healthy habits and behaviors. Your children are watching what you do. If they come to you for help and you’re not utilizing the advice you’re giving them, they’re not going to believe what you say. They’ll revert to poor habits
- Find ways to engage in healthy activities. Talking is great, but actions are also important. Without activities, children may fall into an idle mindset, where they’re entertained and informed by the world or whatever they can get access to. Playing games, helping them with homework, and going for walks are all therapeutic opportunities
Mentors/youth workers:
- Understand that you have an opportunity to build a level of trust that youth may not have with their parents. You may be able to get through to the child or young adult a little easier than a parent or caregiver. Utilize that
- Similar to parents, model healthy behaviors and be active.
- Keep the mentor-to-mentee power dynamic in play. Many mentors and youth workers slip into friendships with the young people they work with. This isn’t inherently a bad thing, but it can become challenging if you become stuck as a friend instead of an authority figure. This, in turn, hinders the help that the young person can receive. Make sure to let them know, “Hey, I’m an adult, and I’m here to listen and be helpful to you”
Some resources
For pastors:
- Soul Shop for Black Churches is a one-day workshop designed for clergy, staff, lay pastors, and faith-based clinicians in Black churches. The training was developed by the American Foundation for Suicide Prevention to address the rates of suicide within the Black community
- The American Psychiatric Association offers “Mental Health: A Guide for Faith Leaders,” a free resource guide for faith leaders who work with congregation members facing mental health challenges
- Learn more about religious CBT via this training video from the Center for Spirituality, Theology, and Health at Duke University
For parents and mentors/youth workers:
If you or someone you know needs help now, call 988 to reach the Suicide and Crisis Lifeline. The lifeline is available 24 hours a day, seven days a week, and is staffed by trained counselors.
The National Alliance on Mental Illness (NAMI) is a national grassroots organization that supports people and families affected by mental illness. The organization provides free mental health support, educational programming, and a helpline via its state and local chapters.
The Black Emotional and Mental Health Collective (BEAM) connects Black people to Black therapists and provides microgrants to Black and marginalized parents living with mental illness or supporting children living with mental illness.
Black Men Heal is on a mission to remove stigma and eliminate cost to care by connecting Black men with therapists and providing eight free sessions. The nonprofit organization also hosts a virtual weekly meetup to discuss male depression, anxiety, anger management, self-care, and more.
The post Meeting the Mental Health Needs of Black Adolescent Boys appeared first on Child Mind Institute.
]]>The post Elyse Myers Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
Take time for yourself to refocus on what you're doing. Take a breather. Give yourself some rest. It's really, really important.Elyse Myers
About Elyse Myers
Elyse Myers is a writer and comedian who first achieved mainstream recognition as a digital content creator. Deemed “The Internet’s Best Friend,” she continues to serve her audience of more than 6M+ with her relatable stories, hilarious coffee-fueled Q&As, and her ability to find the extraordinary in seemingly ordinary moments — all while creating a space to highlight what makes life joyful, messy, and meaningful.
Elyse draws inspiration from comedy icons like Melissa McCarthy, Chris Farley, Amy Poehler, and Nate Bargatze to share her uniquely heartfelt and hilarious perspective on the world as a mom navigating life with humor and honesty. She acts as an advocate for topics like body image, ADHD, anxiety, imposter syndrome, and mental health, offering an unfiltered and deeply genuine glimpse into her everyday experiences.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Elyse Myers Dares to Share appeared first on Child Mind Institute.
]]>The post Paris Jackson Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
I've struggled with depression for as long as I can remember. And it took me a while before I was finally able to start going to therapy. I've been going twice a week for two years now, and it's completely changed my life.Paris Jackson
About Paris Jackson
Paris Jackson is an American actress, model, and musician. Jackson made her acting debut with a guest-starring role on the Lee Daniels Fox series Star. She made her feature film debut opposite David Oyelowo and Joel Edgerton in Gringo and went on to appear in Habit and The Space Between. She most recently starred in Ryan Murphy’s anthology series American Horror Stories and continues to expand her film and television work with new projects in development. Musically, Jackson released her debut solo album with Republic Records and followed it with her 2024 EP The Lost, earning critical praise for her soulful, alternative sound. She is currently touring internationally and working on her highly anticipated second full-length album.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Paris Jackson Dares to Share appeared first on Child Mind Institute.
]]>The post Nikki Reed Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
The more we can talk about it and normalize it the better…Please share your story. There's nothing to be ashamed of.Nikki Reed
About Nikki Reed
Nikki Reed is a prolific actress, designer, and environmentalist. Reed is best known for her portrayal of Rosalie Hale in The Twilight Saga franchise and for co-writing and starring in the critically acclaimed film Thirteen at just 13 years old. She went on to star in several films including Lords of Dogtown and held recurring roles in TV series such as The OC and Sleepy Hollow.
Reed is the Founder and CEO of the socially conscious fine jewelry brand Bayou With Love, which continues to innovate with sustainable and ethical design practices. She also serves as the creative director of the eco-friendly vegan sneaker brand LOCI Wear, represents the iconic camera brand Leica as a photographer, and acts as a strategic advisor for the clean medicine company Genexa. In 2024, Reed expanded her entrepreneurial footprint by launching a new sustainable home goods line under the Bayou With Love umbrella, further solidifying her commitment to eco-conscious living and mindful design.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Nikki Reed Dares to Share appeared first on Child Mind Institute.
]]>The post Maisie Williams Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
Ultimately, just telling someone made me feel better. I didn't even need any big pearls of wisdom. Just being able to express myself helped me get the overwhelming feelings out and they stopped being quite so overwhelming.Maisie Williams
About Maisie Williams
Maisie Williams received critical acclaim and two Emmy nominations for her role as Arya Stark in the smash hit series Game of Thrones on HBO, which released its eighth and final season in April 2019. She then starred in Twentieth Century Fox’s film The New Mutants and the Sky-produced series Two Weeks to Live. She co-hosted the podcast Frank Film Club with Maisie Williams and starred in Danny Boyle’s FX limited series Pistol, which premiered in May 2022. Most recently, Williams earned widespread praise for her portrayal of Catherine Dior in the critically acclaimed Apple TV+ series The New Look, which debuted in 2024. Continuing her work both in front of and behind the camera, she is currently developing new film and television projects through her production company, Rapt.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Maisie Williams Dares to Share appeared first on Child Mind Institute.
]]>The post Keke Palmer Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
About Keke Palmer
Keke Palmer is an Emmy Award-winning actress, producer, and musical artist who rose to prominence through her breakout role in Akeelah and the Bee at age 12 and has gone on to star in over 25 films and 30 TV shows, including STX’s Hustlers, FOX’s Scream Queens, and Nickelodeon’s True Jackson, VP. Palmer recently starred in and executive produced Roadside Attractions’ Alice alongside Common and Jonny Lee Miller, and captivated audiences with her performance in Jordan Peele’s Nope for Universal Pictures. She also lent her voice to the character of ‘Izzy’ in Pixar’s Lightyear. In 2024, Palmer launched her own digital network, KeyTV, aimed at amplifying new creative voices, and continues to expand her musical career with her latest R&B album Big Boss, while earning acclaim for her dynamic performances across film, television, and music.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Keke Palmer Dares to Share appeared first on Child Mind Institute.
]]>The post Steve Aoki Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
Talk! Express yourself, let it out. Share what you're feeling.Steve Aoki
About Steve Aoki
Steve Aoki is an American DJ, record producer, music programmer, record executive, and entrepreneur, as well as the heir to his father Rocky Aoki’s fortune from the Benihana restaurant franchise. In 2012, Pollstar designated Aoki as the highest-grossing electronic dance music artist in North America from tours.
Aoki has collaborated with a wide range of artists, including will.i.am, Afrojack, LMFAO, Linkin Park, Iggy Azalea, Lil Jon, blink-182, Laidback Luke, BTS, Monsta X, Louis Tomlinson, Backstreet Boys, Rise Against, Vini Vici, Lauren Jauregui, and Fall Out Boy, and is widely recognized for his remixes of artists such as Kid Cudi. He has released several Billboard-charting studio albums, notably Wonderland, which earned a Grammy nomination for Best Dance/Electronica Album in 2013. In 2023, Aoki released his highly anticipated album Hiroquest: Double Helix, further cementing his reputation as a boundary-pushing force in electronic music.
He is also the founder of the Aoki Foundation, which supports organizations in brain health research, with a specific focus on regenerative medicine.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post Steve Aoki Dares to Share appeared first on Child Mind Institute.
]]>The post LeAnn Rimes Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
Being able to say, ‘I need help’ and receive that help changed the trajectory of my life and helped to bring me even closer to those who loved me and wanted to help me get to the other side, happier, healthier, and more whole.LeAnn Rimes
About LeAnn Rimes
LeAnn Rimes is an international multi-platinum-selling, acclaimed singer and ASCAP award-winning songwriter who has sold more than 480 million albums globally. She has won 2 Grammy® Awards, 12 Billboard Music Awards, 2 World Music Awards, 3 Academy of Country Music Awards, 2 Country Music Association Awards, and one Dove Award. At 14, Rimes won “Best New Artist,” making her the youngest solo artist to take home a Grammy® Award, and at 15, she became the first country artist to win “Artist of the Year” at the Billboard Music Awards. In 2024, Rimes celebrated the 25th anniversary of her iconic album Sittin’ on Top of the World with a sold-out international tour and continues to garner critical acclaim for her latest album god’s work, which blends country, pop, and spiritual influences. She remains a powerful voice across music and activism, advocating for mental health awareness and holistic wellness.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post LeAnn Rimes Dares to Share appeared first on Child Mind Institute.
]]>The post P!nk Dares to Share appeared first on Child Mind Institute.
]]>Speaking openly about mental health is a courageous step toward connection, healing, and hope. The Dare to Share campaign invites parents, kids, and advocates for young people to share short videos about the mental health challenges they’ve faced and the resilience they’ve built. This May, explore our video library and experience the strength we find when we #DareToShare.
Learn more at Dare to Share.
It does get better. There are beautiful moments waiting for you, and there are beautiful people waiting to love you, and one of those people is yourself.P!nk
About P!nk
Since her debut in 2000, P!NK has released 9 studio albums, 1 greatest hits album, sold over 65 million album equivalents worldwide, achieved 17 singles in the top 10 on the Billboard Hot 100 chart (including four #1 hits), and sold out arenas and stadiums across the globe. She is the recipient of three Grammy Awards (out of twenty-three nominations), one Daytime Emmy Award, seven MTV Video Music Awards including the prestigious 2017 Vanguard Award, two MTV Europe Music Awards, two People’s Choice Awards, was named Billboard’s Woman of the Year in 2013, received The Brits Outstanding Contribution To Music Award in 2019 (as the first international artist honored), and earned a star on the Hollywood Walk of Fame that same year. In 2020, she was honored as Billboard’s Music Awards Icon Recipient, and in 2023, she received the iHeartRadio Icon Award, further cementing her legacy.
Her 2023 studio album TRUSTFALL debuted at #2 on the Billboard 200 and topped charts internationally. The album’s singles, including “Never Gonna Not Dance Again” and “Trustfall,” extended her record with additional #1 hits on Billboard’s Adult Pop Airplay chart. P!NK’s Summer Carnival Stadium Tour, launched in 2023, has become one of the highest-grossing tours of all time, selling over 3.5 million tickets and breaking venue attendance records worldwide.
In addition to her music career, P!NK released her second children’s book, Trustfall: A Story of Letting Go, in 2024, which quickly became a New York Times bestseller. She also continues to expand her work in film and television, with a new documentary project currently in development.
A passionate advocate for social causes, P!NK remains deeply committed to supporting organizations such as No Kid Hungry, Make-A-Wish Foundation, Planned Parenthood, REVERB, Autism Speaks, the Human Rights Campaign.
Speaking up is important, but it can also be hard. These resources can help:
- How to Talk About Mental Health Issues
- How to Help Kids Talk About Learning Disabilities
- How to Talk to Your Parents About Getting Help
The post P!nk Dares to Share appeared first on Child Mind Institute.
]]>The post Black Parents and the Importance of Cultural Competence in Therapy appeared first on Child Mind Institute.
]]>“He was also starting to have a lot of nightmares, and his teacher was calling every week to say that he was disrupting class,” Grace says. “This was not the Denzel I knew. We needed help.”
When Grace contacted her company’s Employee Assistance Program (EAP) for a referral to a mental health provider, she had a few requirements. “I wanted a child psychologist, someone with a practice near enough to go there after school easily, and I wanted them to be Black.”
Finding the first two items on her list was relatively easy, but locating a Black therapist proved much harder. After combing through the list of providers supplied by the EAP, Grace was dismayed to discover that none were Black. “I felt a Black counselor would be a more comfortable fit for Denzel and me,” she says. “I had to insist.” Grace called the administrator of the EAP directly. “The person I spoke with was Black and understood what I wanted,” she says. “It took some doing but we eventually found a Black woman in our area.”
Searching for Black mental health professionals
Finding a Black therapist isn’t easy. According to the 2022 Black Mental Health Workforce Survey, within the United States, only about 5% of psychologists, 7% of marriage and family counselors, 20% of social workers, and 11% of professional counselors are Black. And locating a Black child psychiatrist, specifically, can be even harder. Of the 10,500 child and adolescent psychiatrists currently practicing in the United States, “just 1% are Black,” says Christine M. Crawford, MD, MPH, an assistant professor of psychiatry at Boston University and an adult, child, and adolescent psychiatrist. “If you’re looking for a Black child psychiatrist, especially if you live in the South, Midwest, or a rural area, you’re looking for a unicorn.”
Despite the difficulty, recent research shows that, like Grace, many in the Black community have a strong preference for mental health professionals who look like them and share their cultural beliefs.
A new study conducted by the Child Mind Institute in partnership with the Steve Fund, surveyed 1,000 Black parents seeking care for their child and 500 young Black adults seeking care for themselves. The goal of the study was to garner insight into the experiences and views of Black families and youth around mental health within the United States, as well as identify the key barriers they continue to face. Nearly half of participants (both parents and young adults) said that they trusted a Black mental health professional over one who is white or a non-Black person of color.
“There’s a comfort level that parents get from a Black provider,” says Rhonda Boyd, PhD, associate director of the Child and Adolescent Mood Program at the Children’s Hospital of Philadelphia. “When they feel like they’re understood and can, in turn, understand where the provider is coming from, it can make doing the assessment and understanding the treatment plan easier.”
A question of comfort and safety
There are many in the Black community who still view health care with suspicion. From the Tuskegee syphilis study to the forced sterilization of Black women and girls to the unauthorized harvesting and use of Henrietta Lacks’s cells, there’s a long history of mistreatment and outright racism in the health care system.
“There’s a reason why some in the Black community may not trust the medical establishment,” says Ruth C. White, PhD, MPH, MSW, a diversity trainer and former clinical associate professor in social work at the University of Southern California. “Historically we haven’t been treated well.”
For many, seeing a Black mental health professional can make it easier to put aside these concerns.
As a Black clinician, Dr. Crawford has seen firsthand how her presence affects patients. “There’s a look of relief on the faces of Black parents and caregivers when they meet with me for the first time,” she says. “There’s this sense that they can trust me, that there’s an understanding and an assumption that the diagnosis I provide won’t be rooted in bias or racism.”
This is particularly true when it comes to mental health care for children and adolescents. “There’s often a concern that if your kid were to express any mental health challenges or talk about difficult interactions that they might have with their parents, Child Protective Services is going to be called with that information,” Dr. Crawford says. “That’s how Black families are walking into their encounters with brand new mental health providers because of their life experience.”
Dr. White notes that Black parents may also be wary that receiving counseling for their children may expose them to systemic racism. “It’s important to understand that, historically, Black kids who were reported to have behavior problems were shunted to programs and tracked,” she says. “Parents may resist therapy because they don’t want their kids to get labeled.”
Cultural awareness affects quality of care
Nearly half of the participants in the Child Mind Institute study stated that white and non-Black POC mental health professionals often misunderstand or underestimate the effects racism can have on mental health. “Experiencing microaggressions and racism can lead to racial trauma which, in some people, can elicit symptoms that meet diagnostic criteria for PTSD,” Dr. Crawford says. “When a clinician minimizes or invalidates their experiences, it can create a barrier to wanting to engage in treatment.”
And sometimes the issue is really a lack of cultural awareness. “Clients have told me when they’ve tried to talk about racism with a non-Black provider, it seemed to make the clinician very nervous.” Dr. White says. “And often, clients feel like, now I have to educate my therapist, that’s not what I came here for.”
That’s the situation Danielle D., a paralegal in East Orange, New Jersey, found herself in when she began seeing a white therapist she found through her school. “I remember telling her a story about my mom, and she reacted more stunned and enchanted to hear certain stories about growing up in a Caribbean household,” Danielle says. “She wasn’t derogatory or condescending, but I needed her to act like my therapist and not like a student I was teaching about my culture.”
Instead of being supported, Danielle felt let down. “She really couldn’t understand anything with regards to my family’s background, so I spent most of the time giving in-depth explanations about things a Black therapist would just get,” she says. “I met with her a handful of times before I stopped going and focused on finding a Black therapist.”
And after conducting a lengthy search, Danielle found a Black therapist near her. “Finding someone I can relate to and who could relate to me was key,” says Danielle. “With my other therapist, I just felt like I wasn’t being seen.”
Help finding Black mental health practitioners
Locating a Black therapist may feel challenging, but there are some resources and strategies you can use to simplify the process. A good first step is to leverage your workplace resources, such as your company’s EAP. “It doesn’t hurt to ask them for help identifying Black clinicians,” Grace says. “Don’t overlook your health insurance company,” adds Dr. Boyd. “Ask if there are Black therapists available under your plan.”
If you don’t have access to an EAP, check out websites that provide directories of Black therapists. The following list is a good place to start your search:
- The Association of Black Psychologists
- Black Therapists Rock
- Clinicians of Color
- Inclusive Therapists
- InnoPsych
- Melanin & Mental Health
- Therapy for Black Girls
Once you decide that you’d like your therapist to be Black, it helps to think about what else you’re looking for. For instance, after Danielle narrowed down her search to a Black woman, she also looked for who saw clients in person and who was located within reasonable travel distance from her home. Then she began to comb through directories and asked friends for recommendations.
And if you know of a therapist who might not be right for your situation — say they specialize in couples counseling and you need someone who works with children — consider asking them for a recommendation. Clinicians often have a professional network and can guide you toward trusted practitioners. “Black Therapists Rock has over 20,000 members on its Facebook page,” says Dr. White. “People post saying they are looking, say, for a therapist who deals with Black adolescents in the Washington D.C., area, and members are happy to post referrals.”
Finding culturally inclusive non-Black clinicians
But given the deficit in Black mental health professionals in the United States, the best option may be a carefully chosen non-Black therapist. “I tell folks, do not let the color of your clinician’s skin be the barrier that keeps you from getting the help that you or your child needs,” says Dr. Crawford.
So, if you’re unable to find a Black provider, try to find a non-Black one who is inclusive and culturally sensitive. Changes in the way mental health professionals are taught and trained over the past decade are making this easier. “As someone who oversees the training programs for licensed mental health counselors, psychologists, and psychiatrists, I can tell you providing culturally competent care to people who aren’t of your same background is a required part of training,” Dr. Crawford says. “They’re trained on how to ask questions coming from a place of curiosity, rather than making assumptions or judgments about a patient based on the color of their skin.”
When meeting with any clinician for the first time, it can be helpful to come prepared with questions about their approach to therapy and what you can expect from a typical session. And when dealing with a non-Black therapist, asking about their experience in treating Black patients is key. “Ask explicitly if they are comfortable talking about race and racism and any issues that are important to you, and notice how they react,” says Dr. White. “If the question makes them squirm, if it gives them pause, if they display discomfort, then they may not be the right person for you.”
Dr. Crawford says when it comes to evaluating a non-Black therapist for your child, consider the artwork in the office, what books are on the shelves, and the color of the dolls in the room. “Ask yourself if this is an environment that communicates that all are welcome.”
Once you’ve chosen a clinician, remember those initial sessions with any mental health provider, no matter their race, can feel uncomfortable. “They’re asking a lot of questions and prying into very personal information in a way that may make you feel uneasy,” says Dr. Boyd. “It’s important that you give it a chance.”
Check in with your child regularly about their comfort level with the provider and schedule regular meetings with the provider to make sure everyone is on the same page. And after some time, if you feel like your kid doesn’t feel comfortable, you’re not seeing progress, or you’re unhappy with your interactions, have an open conversation about whether they’re still a good fit. “Therapists are trained to navigate these conversations,” Dr. Crawford says. “And parents should feel empowered to be active participants in their child’s mental health treatment.”
The post Black Parents and the Importance of Cultural Competence in Therapy appeared first on Child Mind Institute.
]]>The post Mom’s Intuition Led Family to Answers appeared first on Child Mind Institute.
]]>So, in second grade I put him back in public school and stressed the fact that he hadn’t written all year. But his writing continued to be a huge problem. We did workbooks at home, but it didn’t make a difference. By the time he was in fourth and fifth grade, we couldn’t understand anything he’d written. There were all these spelling errors, and his handwriting was literally like chicken scratch.
During all that time, he went to martial arts three to four times a week. By middle school, he was a red belt, which comes with lots of responsibility —– he even had his own students. So, it wasn’t just physically challenging, it was also mentally challenging for him. It’s been an incredibly positive part of his life.
During sixth grade, two things happened. Gabriel started to get a lot of coursework, and since his school had sports programs for free, I cut back on martial arts and let him choose some school sports to do instead. But at school activities he wasn’t encouraged to push himself. He would come home and say, “I’m not really doing anything.”
“By the time he was in fourth and fifth grade, we couldn’t understand anything he’d written. There were all these spelling errors, and his handwriting was literally like chicken scratch.”
At the same time a lot of his friends started taking ADHD medications. Gabriel began asking for medication, saying that he was having a hard time focusing. I told him, “No, absolutely not. Your friends have ADHD diagnoses.” Gabriel did not have any diagnoses at that time. He had never even been evaluated. He wasn’t getting in trouble, and his grades were great even though he had trouble writing.
I know ADHD is real, but I also feel like hyperactivity means a kid wants to be active. I felt like his decrease in physical activity was the reason he was saying, “Oh, I’m anxious. Oh, I have ADHD. Oh, I need medication to solve this problem.” But I wanted to make sure I was listening to him and wasn’t just telling him no because I didn’t want him on drugs. I knew that seventh and eighth grade are a time of transition. If Gabriel needed coping mechanisms, I wanted to give him effective ones, and not just say no and have a problem that I was ignoring.
I really wanted to make sure Gabriel didn’t have an attention problem. Ultimately, it was the possibility that there was something else going on in the background that led me to the Healthy Brain Network.
One of my friends who had done the program suggested the Healthy Brain Network to us to make sure there was nothing else going on. She knows Gabriel well, knew he had a lot of anxiety when he was younger, and that he seemed very introverted even though that wasn’t necessarily his natural tendency. She told me, “Just sign up and see what they come back with.”
When we got our feedback report, I was really happy to finally get words for problems that we had been experiencing — to be able to explain the disconnect between home and school.
We participated when he was 14, and our experience was pretty good. It’s been great for Gabriel actually. It was so good for Gabriel’s ego. He liked that the staff loved how fit he was. He flew through a lot of the physical challenges, and he exceeded expectations. He loved the energy and the effort.
When we got our feedback report, I was really happy to finally get words for problems that we had been experiencing — to be able to explain the disconnect between home and school. The two big takeaways were that he had executive functioning issues and he lacked the motor skills to write properly.
It was validation for a lot of —– for lack of a better word —– my paranoia. His handwriting was illegible; he had strong ideas, but his writing lacked cohesion since he waited until the last minute to do things. I had been reaching out to teachers about it and their response was, “Ahh, boys… that happens from time to time with boys. It’s fine.”
“We’ve found a tutor for executive functioning. He’s been doing that for several months now. And it’s been making impacts in his life.”
The clinician recommended that he get an assisted writing device, such as a tablet, and a 504 plan, saying that he needs an assisted device in school. It was helpful because we were able to take that to the school, to his counselor and teachers, and say, “These are challenges that he has, and these are steps that we’re taking outside of school to help with it.”
We’ve found a tutor for executive functioning. He’s been doing that for several months now. And it’s been making impacts in his life. The extra support is supposed to get him to work on the things that he doesn’t want to do. He has a whiteboard in his room, and I see him writing out lists of things that are important to him. He’s setting goals and priorities, verbalizing them and putting them in order.
There are still challenges. Tardiness is a challenge, but he’s definitely aware of it. And we’re in communication with the school about it. It’s still a journey to incorporate these things in life.
And I’ve seen him clean up his room on his own. Some 16-year-olds might do this, but he’s never been one of those people. Lately he takes initiative and cleans up his room. That is a positive change: seeing him using those tools in areas where he needs it.
The post Mom’s Intuition Led Family to Answers appeared first on Child Mind Institute.
]]>The post A Mother’s NVLD Journey appeared first on Child Mind Institute.
]]>Because nonverbal learning disability is not in the DSM, my daughter did not receive an optimal education. Schools and educators often did not understand her because NVLD is not recognized as an official diagnosis. This makes it difficult for children with NVLD to receive appropriate accommodations in school and empathic understanding that is critically important to one’s development.
Because nonverbal learning disability is not in the DSM, my daughter did not receive an optimal education.Laura Lemle, PhD
This population often does not read nonverbal social cues accurately. Misreading social cues can be annoying to both adults and children. However, understanding why an individual is behaving in an off-putting way can potentially be used as a teachable moment. Instead, too often, individuals with NVLD are stigmatized and ostracized. Being accepted socially and feeling supported by a community remain among the biggest obstacles.
My daughter’s unwavering determination and courage inspired me to want to do something to help this community. I talked to a lot of people, tried a few things, and then in 2012, I realized the way that I could most effectively help this population was to try to get NVLD recognized as a formal disorder. In 2013, I founded The NVLD Project, a nonprofit organization dedicated to raising awareness, building support, and furthering our understanding of this disability. I want to help others on this journey who might feel isolated and alone because I know the importance of belonging to a community and I know how challenging it can be to find the resources necessary to help your child succeed. I was and am also concerned about the adult community. Children grow up and their disability follows them. Having nonverbal learning disability recognized by the Diagnostic and Statistical Manual Committee (DSM) as a valid disorder will be a game changer.
My daughter’s unwavering determination and courage inspired me to want to do something to help this community.Laura Lemle, PhD
In a relatively short time, we have made considerable strides. Through our partnership with researchers at Columbia University Medical Center, an application was submitted to the DSM Committee to get NVLD recognized as a formal disorder under the new name Developmental Visual Spatial Disorder. (Research is now being done at Child Mind Institute and Columbia using the new criteria to resubmit the application to the DSM committee at their request.) We funded the first stand-alone clinic for assessment and treatment of NVLD at Ferkauf Graduate School of Psychology at Yeshiva University, the Lemle Clinic. We are also very excited about our new and very important partnership with Child Mind Institute. They are focusing on NVLD research as well as clinical care and assessment for this population.
I am very pleased and grateful that our organization is working with some of the most prominent experts in the field, including researchers, psychologists, psychiatrists, educators, and their renowned institutions. Thanks to the support of so many individuals and organizations, my passion for providing much needed help and resources to others with NVLD and their families is becoming a reality. While I am extraordinarily proud of what we have accomplished so far, I do realize that in many ways our work has just begun.
Please join me and all of us at The NVLD Project in our critically important work to obtain a valid diagnosis for Nonverbal Learning Disability so that those living with this disability can be better understood, properly treated, socially engaged, and counted in.
The post A Mother’s NVLD Journey appeared first on Child Mind Institute.
]]>The post New Study Published in The Lancet Global Health Reveals Significant Data Gaps About Mental Health Conditions of Children Around the World appeared first on Child Mind Institute.
]]>New York, NY — A landmark new study led by investigators from the Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute, United for Global Mental Health, and the Global Mental Health Action Network, highlights critical data gaps in mental health conditions, particularly for children in low- and middle-income countries, with the largest gaps documented in the Western Pacific and Africa.
The study will be published on April 24, 2025, in The Lancet Global Health with the title “Data Gaps in Prevalence Rates of Mental Health Conditions Around the World: A Retrospective Analysis of Nationally Representative Data.” It aims to quantify and analyze the distribution of the available nationally representative prevalence data for mental health conditions.
Reflecting on the study’s significance, Giovanni Salum, MD, PhD, the senior vice president of Global Programs at the Child Mind Institute and senior author of the study, emphasized its implications for global youth mental health advancement and advocacy.
“Through this collaboration, we’ve gathered evidence that marks a pivotal moment in our understanding of global mental health data gaps while providing a foundation for change through coordinated efforts. As we continue to lead critical discussions on global youth mental health — and ahead of the United Nations General Assembly in September, where accelerating action to improve mental health will be a top priority — our findings provide a clear road map to strengthen systems and inform policy,” said Dr. Salum. “By combining open science frameworks with enhanced data collection and cross-sector partnerships, we can reduce the knowledge gap.”
Despite increased interest in and availability of data for mental health overall since 2000, the growth in scientific research was found to be the lowest on the topic of children’s mental health. Furthermore, most of the available datasets were collected prior to 2010 and may not reflect current challenges and needs. This also points to a stark reality: Low and middle-income countries are the hardest hit in terms of data gaps, creating an urgent need for solutions — a challenge this paper directly addresses.
Improving data collection and research, while advocating for targeted policy action, is essential in bridging the data gap, which can perpetuate stigma and hamper sustainable transformation.
Antonis Kousoulis, MD, director of partnerships at United for Global Mental Health and the Global Mental Health Action Network lead, reiterated the need for strengthened systems.
“We are excited to support this new research and policy brief. In a year when the global mental health sector is working hard to influence the United Nations High-Level Meeting on non-communicable diseases and mental health, it is concerning that our research in partnership with the Child Mind Institute highlights extensive global data gaps, an absence of up-to-date mental health datasets, and a scarcity of credible indicators. Having timely, representative, and high-quality data on mental health is essential to provide an evidence base for decision-making, drive policy change, ensure accountability, and make the case for increased investment and improved access to services,” said Dr. Kousoulis.
Currently, more than 80 percent of countries and territories worldwide have no recent data on the prevalence of mental health conditions. There are no nationally representative data sources for children in Africa. And while child mental health was most covered in the Eastern Mediterranean Region and in the European Region, it was still insufficient, with only 23 percent and 21 percent, respectively, of their countries having at least one data source.
Mental health conditions are among the leading contributors to disability and illness globally, negatively affecting quality of life and academic and professional performance. This study therefore underscores the vital role of global partnerships in improving data collection on healthcare, social, economic, and environmental factors, to help identify underlying causes and culturally relevant preventative measures.
Good data are critical for policy makers. Analyzing the true extent of these problems is essential to guide resource allocation, advocacy, monitoring mental health trends, and ultimately improving population health.
This work is conducted by the Stavros Niarchos Foundation (SNF) Global Center at the Child Mind Institute with founding support from the Stavros Niarchos Foundation (SNF) as part of its Global Health Initiative (GHI).
About the SNF Global Center at the Child Mind Institute
The SNF Global Center brings together the Child Mind Institute’s expertise as a leading independent nonprofit in children’s mental health and the Stavros Niarchos Foundation’s (SNF) deep commitment to supporting collaborative projects to improve access to quality health care worldwide. The center is building partnerships to drive advances in under-researched areas of children’s and adolescents’ mental health and expand access to culturally appropriate trainings, resources, and treatment in low- and middle-income countries. This work is conducted by the Child Mind Institute with support from SNF through its Global Health Initiative (GHI).
About the Child Mind Institute
We are the leading independent nonprofit in children’s mental health providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing open science initiatives and tomorrow’s breakthrough treatments.
About United for Global Mental Health
United for Global Mental Health is an advocacy organisation working with partners across the world to raise awareness, reduce stigma and increase support for mental health across the world. Our vision is for a world where mental health support is accessible to everyone, everywhere without stigma or discrimination. UnitedGMH’s work on this is supported by Flourishing Minds and the Wellcome Trust, and by its role in the Being Initiative.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post New Study Published in The Lancet Global Health Reveals Significant Data Gaps About Mental Health Conditions of Children Around the World appeared first on Child Mind Institute.
]]>The post Vaccines and Autism: A Clinical Perspective appeared first on Child Mind Institute.
]]>What is autism?
Autism, or autism spectrum disorder (ASD), is a neurodevelopmental disorder, meaning it impacts the development of the brain. Autism is characterized by impairment in social communication skills — a technical way of saying that it affects the way a child engages in conversation, makes friends, and reads social cues. Kids on the autism spectrum also exhibit restricted and/or repetitive behaviors and interests, often called RRBs for short. These can include repetitive movements and use of objects — hand flapping, lining up toy cars, or sorting crayons by color. RRBs can also include strong special interests in very specific topics or things, like sports, transit systems, numbers, anime, or water.
Research suggests that autism may be present in a child before they are born, although it does not fully emerge until the toddler stage at the earliest. And people can be diagnosed with autism at any age. Perhaps their symptoms or autistic traits were harder to see when they were younger, they didn’t meet all the diagnostic criteria yet, or it was overlooked entirely. People with autism have a wide range of social skills and behaviors — that’s why it’s called a spectrum.
Cynthia Martin, PsyD, the senior director of the Autism Center at the Child Mind Institute, says that individual presentations of autism — i.e., how individual autistic people behave and engage with the world — are so diverse that it might actually be more accurate to say “autisms” rather than putting everyone in one big category.
To be diagnosed with autism, a child’s challenges with social communication skills and RRBs must impact their daily functioning in ways that require some degree of support. For some kids, support means accommodations in school or seeing a therapist a few times a week; for others, it means round-the-clock help with basic personal care.
Do vaccines cause autism?
No. After the publication of more than 20 research studies directly examining the claim, there remains no scientifically acceptable evidence that vaccines cause autism. But it’s helpful to understand where the idea came from and why people have singled out the MMR vaccine in particular.
What is the MMR vaccine?
The MMR vaccine is a combination vaccine that provides immunity against three exceptionally dangerous and life-threatening diseases: measles, mumps, and rubella. It was developed in 1971.
Before a vaccine was available, almost all children contracted measles before the age of 15. The disease killed 1–2 children out of 1,000, and there is no specific treatment for it. Meanwhile, exposure to rubella during pregnancy can cause miscarriages, stillbirths, and serious birth defects. Mumps is less deadly but can cause swelling around the brain and lifelong complications, such as deafness.
The MMR vaccine protects individuals from contracting these diseases and in doing so, protects the larger community. Take measles, which has an astonishing 90% infection rate. Even a few people without immunity can cause a population outbreak. (Two doses of the MMR vaccine are 97% effective in preventing measles; one dose is about 93% effective.) Low immunization rates — driven in part by parents choosing not to vaccinate their children — led to a 20% increase in measles cases worldwide between 2022 and 2023.
The Wakefield report and the roots of MMR vaccine suspicion
In 1998, then medical doctor Andrew Wakefield published an article in the Lancet, a respected medical journal. In it, he claimed evidence that the MMR vaccine could cause symptoms of autism in children. But the paper was seriously flawed. Further investigations found that Wakefield had manipulated and even falsified data in addition to other serious ethical violations — all of which were later acknowledged by the Lancet.
The Wakefield paper was based on case reports of 12 children. This is important because 1) valid studies need to involve a lot more participants to demonstrate significance and even more to appropriately represent the larger population; and 2) a case report isn’t actually a study. Case reports provide detailed medical histories for individual patients. They can be very useful for collecting data — or for pointing to an issue worthy of further study — but they’re not built to support claims on their own.
In 2010, the independent British General Medical Council (GMC) found Wakefield guilty on 30 charges of professional misconduct. The council was particularly outraged by his “callous disregard” for the report’s child participants and his misrepresentation of their symptoms. They also cited him for various ethical violations, noting that his research was paid for in part by lawyers seeking to sue vaccine makers. The Lancet retracted the article, and Wakefield lost his medical license.
Meanwhile, other researchers tested Wakefield’s claim. Dozens of reports were published, including two consecutive studies involving every child born in Denmark over a 30-year period. None could find any link between the MMR vaccine and autism.
Why MMR vaccine suspicion persists
Wakefield and his report received a lot of media attention, creating a link between vaccines and autism in public thought. The claim was so ubiquitous that, regardless of your opinion, it was likely you had heard it. And for some, the link seemed to make sense because of coincidence. Signs of autism typically begin to appear between the ages of 0 and 2 because doctors, caregivers, and parents are tracking a child’s social-communication milestones — making eye contact, using hand signals, responding to their name — in real time. This is also around the time it’s recommended that kids receive the first dose of the MMR vaccine.
“If you see things happening to your child right next to each other, it’s a normal parenting instinct to be like, ‘Oh, there should be some link,’” says Dr. Martin, who is also a parent.
Once the association between the MMR vaccine and symptoms of autism had been made, people understandably thought they saw “evidence” that one had caused the other — which can be a powerful personal motivator, even when all scientific evidence shows that the two events are unrelated. But what parents saw was correlational (when two things happen at the same time) not causal (when one thing causes another).
But what about the ingredients in vaccines?
There is no reason for concern about ingredients in vaccines — and scientists aren’t saying that lightly. Vaccine opponents often single out a preservative containing mercury called thimerosal as a cause for alarm. The Federal Food and Drug Administration (FDA) asked companies to remove thimerosal from vaccines beginning in 1999 as a precaution, and since then, dozens of studies have shown it to be safe. But in 2000, several parent groups raised the claim that thimerosal caused autism.
Researchers embarked on dozens of studies and examined decades worth of data across multiple countries to test the claim. They could not find any link between vaccines, thimerosal, or mercury and autism. Mercury sounds terrifying, but to be clear, thimerosal contains a small and safe amount of the same variety found in fish — and about as much of it as you would find in a three-ounce can of tuna.
More importantly, the MMR vaccine never contained thimerosal to begin with.
What causes autism?
The honest answer is we don’t fully know right now — but here’s a little background about what we’ve learned about autism and a snapshot of where the research currently stands.
A brief history of autism
Autism was first identified in the 1940s, but it didn’t become a formal diagnosis until it appeared in the Diagnostic and Statistical Manual of Mental Disorders, the DSM-3, in 1980.
The definition was revised to include more criteria for diagnosis in 1987, and it has further expanded in subsequent versions of the manual. The most current version, the DSM-5, now includes under autism some disorders that had been previously categorized separately. For example, Asperger’s Disorder was once a separate diagnosis but is now consolidated into autism spectrum disorder.
In 2000, 1 in 150 children in the United States were diagnosed with autism. In 2025, the CDC reported it was 1 in 31.
When clinicians see the figure from the CDC, it tells them that more children are being diagnosed with autism by a doctor or being classified as having autism on their school IEP because of the way the statistics are calculated. In the past, lots of people who had autism weren’t diagnosed, so they weren’t captured in the statistics. And parents and clinicians are getting better at recognizing autism at different ages and getting kids diagnosed so they can get the help they need.
Potential causes of autism: genetic and environmental
As our understanding of autism rapidly evolves, so does genetic research into its causes. “When I was a medical student, there were just a few genes known to be involved with autism,” says Adriana Di Martino, MD, the founding and research director of the Autism Center at the Child Mind Institute. Today, researchers have identified over 100 — evidence that there are multiple causes, and likely pathways, involved in how autism develops.
Autism is thought to arise from a complex interplay of factors that influence early brain development. These include genetic, prenatal, and, to some degree, environmental factors.
Genetic contributions include heritability, rare mutations, and common polygenic variations (meaning there are multiple genes that contribute to autism susceptibility). Various prenatal and environmental factors that have been implicated in an increased likelihood of autism include advanced parental age, particularly older fathers; maternal infections; toxin exposures; metabolic conditions during pregnancy; and birth complications.
Clinicians emphasize the importance of autism awareness, education, and early intervention. Because the earlier a child is diagnosed, the earlier they can start receiving support.
“We need to get kids diagnosed as early as autism symptoms become detectable,” Dr. Martin says. “Then we need to have individualized and well-tailored interventions that are meaningful and make sense for that child. And support them in having the best quality of life possible.”
Frequently Asked Questions
No, vaccines do not cause autism. More than 20 rigorous, high-quality studies have found no evidence to support this claim.
There is evidence that there are multiple causes, and likely pathways, involved in how autism develops. Autism is thought to arise from a complex interplay of factors that influence early brain development. These include genetic, prenatal, and, to some degree, environmental factors during gestation.
The MMR vaccine is a combination vaccine that provides immunity against three exceptionally dangerous and life-threatening diseases: measles, mumps, and rubella.
The post Vaccines and Autism: A Clinical Perspective appeared first on Child Mind Institute.
]]>The post Schizophrenia Test appeared first on Child Mind Institute.
]]>Schizophrenia is a serious mental health condition that can cause people to lose touch with reality and see, hear, or believe things that aren’t real or true. It is usually diagnosed in late adolescence or early adulthood, but symptoms of schizophrenia can appear earlier. There is no simple schizophrenia test, but our resources and Symptom Checker can be a good first step on the road to diagnosis and treatment.
What is schizophrenia?
Schizophrenia is a mental health disorder that affects an individual’s ability to distinguish reality from fantasy. People with schizophrenia can experience psychosis in the form of hallucinations (hearing voices or seeing things that aren’t there) or paranoid delusions (thinking that someone or something can read their mind or is trying to hurt them). These symptoms can disrupt their social interactions, academic performance, and overall ability to function.
While schizophrenia is most commonly diagnosed in the late teens or early adulthood, signs can emerge earlier, particularly in the teen years when development and stressors can bring out underlying mental health issues. While rare, it can also develop in children.
Take our schizophrenia test
If you’re looking for a free schizophrenia test, you can use our Symptom Checker to help you determine if your child or teen might have schizophrenia. If you answer a series of questions about your child’s behaviors, the Symptom Checker will let you know if they correspond with the symptoms associated with schizophrenia. If your answers to the quiz suggest another disorder, you’ll see that, too.
How accurate is our online schizophrenia test?
The Symptom Checker was developed in partnership with expert clinicians and is aligned with the Child Mind Institute’s rigorous editorial standards and the latest Diagnostic and Statistical Manual (DSM-5).
If you think your child may have schizophrenia or another mental health disorder, it’s important to get a diagnosis from a medical or mental health professional. But if you’re looking for an online schizophrenia test to get started, our Symptom Checker can help you know if the behaviors you notice in your child correspond with signs of schizophrenia, or something else. You’ll also find links to articles where you can learn more about schizophrenia and help you prepare for a conversation with a professional who can diagnose your child.
Schizophrenia symptoms
Kids with schizophrenia have strange, often concerning thoughts and behaviors. Early signs of schizophrenia in children and teens can include:
- Ideas that don’t make sense: They may believe they have superpowers, think others want to hurt them, believe that strangers know them or are talking about them, or that TV shows are sending them special messages.
- Psychosis: They may see, hear, or feel things that aren’t there. Voices may tell them what to do, often in a threatening or scary manner.
- Withdrawal from friends and family: There may be a noticeable decline in their social interaction and withdrawal from activities they previously enjoyed.
- Changes in behavior or personality: You may notice a shift in your child’s personality, such as becoming unusually anxious, suspicious, or paranoid.
- Strange speech or thoughts: They may demonstrate disorganized speech or thinking, such as jumping from topic to topic with little coherence, or speaking in a way that doesn’t make sense to others.
- Decline in academic performance: A sudden drop in school performance or an inability to concentrate and complete tasks may be an early indicator.
It’s important to differentiate between common teenage struggles like mood swings and more serious mental health issues like schizophrenia. If these changes are persistent and worsening over time, it may be a sign of schizophrenia or another mental health disorder.
Why can schizophrenia be hard to detect in children and teens?
Early onset schizophrenia is rare, so symptom in children can be overlooked, hidden, or confused with other conditions. Changes can be gradual and thus difficult to detect. A child may appear to have attention issues since they are so distracted by internal stimuli like delusional thoughts. Or they may appear anxious generally, when their anxiety is in fact a response to scary hallucinations. Kids experiencing these symptoms may also experience disrupted sleep, increased irritability, or deteriorating grades. And because these symptoms can be confusing or embarrassing, children may be hesitant to share. Since schizophrenia in is rare in children, parents are often more likely to assume their child has ADHD, anxiety, or depression, or is just being rebellious.
In teenagers, early signs may be overlooked until the teen has a psychotic episode, and their behavior becomes disturbing or dangerous. Teens having a psychotic episode may end up in the ER, as parents worry that they aren’t safe, or be arrested because their behavior is erratic or harmful to others.
Teens with schizophrenia are sometimes misdiagnosed with bipolar disorder because their unusual behavior during a psychotic episode can be confused with the mania that is part of bipolar disorder.
How is schizophrenia different from bipolar disorder?
People with schizophrenia may experience episodes of psychosis, with periods of normal behavior in between. Bipolar disorder, which also develops during the teenage years, involves episodes of both depression and mania, lasting for weeks or months. However, some individuals can have schizoaffective disorder, in which they experience symptoms of both.
What causes schizophrenia?
The exact cause of schizophrenia is not fully understood, but research suggests that it is a combination of genetic and environmental factors. Children with a family history of schizophrenia or other mental health disorders are at a higher risk of developing the condition. Environmental factors, such as trauma or exposure to drugs or alcohol, may also contribute to the onset of schizophrenia.
It is important to note that schizophrenia is not caused by anything the child or family has done wrong — it is a medical condition that requires treatment and support.
When can you test a child for schizophrenia?
You should seek professional psychiatric attention at any age if you have concerns about your child’s mental health. While schizophrenia is not typically diagnosed until the teenage years, schizophrenia in children is rare but possible.
How is schizophrenia diagnosed?
Before diagnosing schizophrenia, a mental health professional will rule out other possible causes of the concerning behavior. This includes drug or alcohol abuse, underlying medical issues, and other mental health problems.
Schizophrenia is diagnosed via a thorough evaluation by a mental health professional, typically a psychiatrist. The process includes:
- Clinical interviews: Discussions with the child, parents, and other caregivers to understand the child’s behaviors, thoughts, and emotional state.
- Medical and psychological assessments: These can include a series of tests or observations to rule out other possible conditions and determine if the symptoms meet the criteria for schizophrenia.
- Family history: The doctor will ask about any family history of schizophrenia or other psychiatric conditions, as genetics can play a role in the development of the disorder.
There is no single schizophrenia test, but a combination of interviews, observations, and evaluations will help the doctor make an accurate diagnosis.
How is schizophrenia treated?
While schizophrenia is a lifelong condition, treatment soon after the first psychotic episode can dramatically improve outcomes, reducing the likelihood or frequency of later episodes. The recommended treatment is called Coordinated Specialty Care, which teaches kids how to deal with their symptoms. The treatment includes:
- Medication: Antipsychotic medications are typically prescribed at lower doses than in standalone medication treatment for schizophrenia. The medication helps reduce the symptoms of psychosis, such as delusions, hallucinations, and disorganized thinking. Finding the right medication and dosage can take time and may require regular adjustments.
- Therapy: Cognitive behavioral therapy for psychosis (CBTp) helps children and teens manage the emotional and psychological challenges of schizophrenia.
- Educational support: Teens who have had a psychotic episode get support for returning to school and accommodations at school, such as an Individualized Education Program (IEP), if needed to help them succeed academically.
- Family support: Families get coaching on how to help kids who have schizophrenia keep appointments, take their medications, and stay healthy. Things like eating well and sleeping enough are important because stress can trigger a relapse. Parents also learn how to respond when their child is having delusions, and how to manage a crisis.
How much does our online schizophrenia test cost?
The Symptom Checker is a free-to-use test that can help you identify possible signs of schizophrenia or other mental health disorders. It is not an official diagnostic tool but can be a first step in your journey.
Frequently Asked Questions
Schizophrenia is a mental health disorder that makes it hard to tell what’s real. It often involves hallucinations (like hearing voices) and paranoid delusions (believing someone is trying to harm them). It usually appears in late teens or early adulthood, but can also develop in children.
Symptoms include confusing or strange beliefs, hallucinations, withdrawal from others, sudden personality changes, disorganized speech, and declining school performance. These behaviors can be mistaken for anxiety, ADHD, or depression, especially in children and teens.
A mental health professional diagnoses schizophrenia through interviews, behavioral assessments, and a review of medical and family history. There’s no single test — diagnosis is based on observing patterns and ruling out other causes.
Further Reading
The post Schizophrenia Test appeared first on Child Mind Institute.
]]>The post The Second Cohort of Stavros Niarchos Foundation (SNF) Global Center Clinical Fellows From Mozambique Arrives in Brazil for Child Mental Health Training appeared first on Child Mind Institute.
]]>Porto Alegre, Brazil — The Stavros Niarchos Foundation (SNF) Global Center for Child and Adolescent Mental Health at the Child Mind Institute and the International Association for Child and Adolescent Psychiatry and Allied Professions (IACAPAP) are proud to welcome the second cohort of clinical fellows from Mozambique for advanced training in child and adolescent mental health in Brazil.
The new cohort — psychiatrist Anibal Anube, MD; psychologist Paulino Feliciano; and occupational therapist Florentino Costume — arrived in Porto Alegre in March 2025. The fellows will spend the next year training at the Hospital de Clínicas de Porto Alegre (HCPA) under the supervision of leading clinicians before returning to Nampula in northern Mozambique for an additional year of training and preparation as a multidisciplinary team to strengthen child and adolescent mental health services in the public sector.
At the same time, the first cohort of fellows — psychiatrist Carmen Rungo, MD; psychologist Cristina Lopes; and occupational therapist Custodia dos Anjos, occupational therapist — are returning to Maputo, the capital of Mozambique, to begin their second fellowship year. There, they will continue their training in clinical service delivery, working collaboratively as a team to support children, adolescents, and families in the public health system.
In March, representatives from the SNF Global Center traveled to Porto Alegre to meet with all six fellows, tour the training facilities, and strengthen collaboration with IACAPAP and local partners. The team also visited the Hospital de Clínicas de Porto Alegre, the site of clinical training, and held coordination meetings with IACAPAP leadership.
“Collaborating to develop child and adolescent mental health services and expertise in underserved regions is core to IACAPAP’s mission,” said Luis Rohde, MD, PhD, president of IACAPAP. “We could not be happier with the initial results of this initiative. We are confident that this remarkable group of fellows will make a meaningful difference in Mozambique and that the program will serve as a strong model for the region.”
“It is a pleasure to welcome the second group of the program here at Hospital de Clínicas de Porto Alegre,” said Virginia de Oliveira Rosa, MD, PhD who oversees the fellows’ training at HCPA. “We are deeply motivated by this program, and our goal is to ensure that the care the fellows provide upon returning home is both effective and culturally relevant.”
The fellowship is part of a larger initiative by the SNF Global Center to train mental health professionals from low- and middle-income countries, with a focus on building national capacity through long-term mentorship and training. The program was designed in collaboration with the Mozambique Ministry of Health, which is deeply invested in expanding access to care for children and adolescents.
“I greatly appreciate the way in which the Mozambican fellows have been — and continue to be — integrated into this clinical fellowship program,” said Lídia Gouveia, MD, PhD, of the Mozambique Ministry of Health. “The commitment of the teams at CAPSi (the Child and Adolescent Psychosocial Care Center) and HCPA to meet the specific needs of each fellow, while also taking into account the challenges they will face in Mozambique, is truly remarkable.”
“I am honored to be part of this program, and proud that Mozambique was selected by the SNF Global Center and IACAPAP to launch it,” said Helena Daniel, MD, PhD, the fellowship coordinator in Mozambique and the country’s first child psychiatrist. “Thanks to this initiative, Mozambique now has two child psychiatrists and a dedicated team — including a psychologist and an occupational therapist — focused on child mental health. The partnership with Brazil and HCPA strengthens our training, broadens our perspectives, and advances mental health care in Mozambique. Investing in childhood is investing in the future — it transforms lives and lays the foundation for healthier generations.”
Dr. Daniel, who trained at HCPA with Dr. Rohde, now mentors all the fellows, including Dr. Rungo, Mozambique’s second child psychiatrist, and Dr. Anube, who will become the third. Together, this growing group of experts is laying the foundation for a national child and adolescent mental health infrastructure in Mozambique.
This innovative partnership between the SNF Global Center for Child and Adolescent Mental Health and IACAPAP reflects a shared commitment to expanding global access to high-quality mental health care for young people. By investing in the training of generalist clinicians in low- and middle-income countries, the program addresses urgent workforce gaps while fostering international collaboration and knowledge exchange. The fellowship model represents a scalable approach that can serve as a blueprint for similar initiatives around the world — offering a powerful example of how local leadership, institutional partnerships, and long-term investment can help build sustainable systems of care for children and adolescents.
To learn more about the fellowship and the SNF Global Center’s work, visit childmind.org/global.
This work is conducted by the Stavros Niarchos Foundation (SNF) Global Center at the Child Mind Institute with founding support from the Stavros Niarchos Foundation (SNF) as part of its Global Health Initiative (GHI).
About the SNF Global Center at the Child Mind Institute
The SNF Global Center brings together the Child Mind Institute’s expertise as a leading independent nonprofit in children’s mental health and the Stavros Niarchos Foundation’s (SNF) deep commitment to supporting collaborative projects to improve access to quality health care worldwide. The center is building partnerships to drive advances in under-researched areas of children’s and adolescents’ mental health and expand access to culturally appropriate trainings, resources, and treatment in low- and middle-income countries. This work is conducted by the Child Mind Institute with support from SNF through its Global Health Initiative (GHI).
About the Child Mind Institute
We are the leading independent nonprofit in children’s mental health providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing open science initiatives and tomorrow’s breakthrough treatments.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post The Second Cohort of Stavros Niarchos Foundation (SNF) Global Center Clinical Fellows From Mozambique Arrives in Brazil for Child Mental Health Training appeared first on Child Mind Institute.
]]>The post The SoFi Child Mind Institute Golf Invitational Raises $700,000 to Support Mental Health Care for Bay Area Youth appeared first on Child Mind Institute.
]]>San Francisco, CA – Notable Bay Area athletes turned out in force to raise funds for youth mental health at the SoFi Child Mind Institute Golf Invitational on April 7, 2025, at the Olympic Club in San Francisco. The athletes—including Marcus Allen (Los Angeles Raiders), Royce Clayton (San Francisco Giants), Vince Coleman (St. Louis Cardinals), Brandi Chastain (U.S. women’s soccer), and Jerry Smith (NCAA champion soccer coach)—spent a day on the links to support the Child Mind Institute’s mission to transform the lives of children and families struggling with mental health and learning disorders.
Alex Smith, a former NFL player and mental health advocate, served as featured dinner speaker and talked candidly about his experiences with anxiety and imposter syndrome early in his professional career. He also spoke about his battles, both physical and mental, following a life-threatening injury.
Raj Mathai, twelve-time Emmy Award winner and weeknight news anchor for NBC in the Bay Area, was on hand as well and served as the dinner program emcee and auctioneer.
Harold S. Koplewicz, MD, president of the Child Mind Institute, remarked, “There are very few truly bipartisan issues in our country today, but one that does unite us all is the growing crisis in youth mental health. It’s a crisis that doesn’t discriminate, affecting children in every community and from every background.”
SoFi was the event’s title sponsor. “Expanding children’s access to mental health and wellness resources is an essential investment in their future and the future of their communities,” said Anthony Noto, CEO of SoFi. “We’re honored to partner with the Child Mind Institute to support families with the tools they need to thrive and realize their ambitions.”
Additional sponsors included Wachtell, Lipton, Rosen & Katz, Gingerbread Capital, TPG, Los Angeles Chargers, Los Angeles Rams, and Hollywood Park, as well as product and vendor support from Bay Golf Club, Dryvebox, Moretz Marketing, SightGlass, Supergoop!, and TGL presented by SoFi. Tracy Toyota served as the event’s Hole-in-One Sponsor.
The SoFi | Child Mind Institute Golf Invitational event committee included Jane Burgess, Stacy Denman, Jake Leschly, Ronnie Lott, Kristin Noto, and Linnea Roberts.
About the Child Mind Institute
We are the leading independent nonprofit in children’s mental health providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing open science initiatives and tomorrow’s breakthrough treatments.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
About SoFi
SoFi (NASDAQ: SOFI) is a member-centric, one-stop shop for digital financial services on a mission to help people achieve financial independence to realize their ambitions. The company’s full suite of financial products and services helps its over 10.1 million SoFi members borrow, save, spend, invest, and protect their money better by giving them fast access to the tools they need to get their money right, all in one app. SoFi also equips members with the resources they need to get ahead — like credentialed financial planners, exclusive experiences and events, and a thriving community — on their path to financial independence.SoFi innovates across three business segments: Lending, Financial Services — which includes SoFi Checking and Savings, SoFi Invest, SoFi Credit Card, SoFi Protect, and SoFi Insights — and Technology Platform, which offers the only end-to-end vertically integrated financial technology stack. SoFi Bank, N.A., an affiliate of SoFi, is a nationally chartered bank, regulated by the OCC and FDIC and SoFi is a bank holding company regulated by the Federal Reserve. The company is also the naming rights partner of SoFi Stadium, home of the Los Angeles Chargers and the Los Angeles Rams. For more information, visit SoFi.com or download our iOS and Android apps.
The post The SoFi Child Mind Institute Golf Invitational Raises $700,000 to Support Mental Health Care for Bay Area Youth appeared first on Child Mind Institute.
]]>The post Beyond the ADHD Headlines: A Nuanced Look at Diagnosis, Drugs, and Daily Life appeared first on Child Mind Institute.
]]>By Michael P. Milham, MD, PhD
Chief Science Officer, Child Mind Institute
A recent New York Times Magazine article by Paul Tough raises questions about the increasing number of children diagnosed with ADHD and the long-term use of medication for the treatment of ADHD. While concerns about possible overdiagnosis of ADHD deserve careful attention, it is equally important to recognize that modern pressures — pandemic stress, relentless academic demands, and a digital culture that rewards constant multitasking — can unmask or worsen ADHD symptoms.
One size doesn’t fit all
ADHD is not a homogeneous condition, as the article rightly stresses. As with many clinical conditions, each child’s genetic, brain-based, and environmental influences blend into a distinct profile. One child might have more impulsivity or hyperactivity that are obvious in the classroom and on the playground. Another might have inattentive traits that they are able, with great effort, to hide. Children also differ in cognitive abilities and in co-occurring conditions they might have. That’s why thorough evaluations — spanning different settings — are vital. We need to rule out other causes of inattention (like anxiety or trauma) and ensure we’re capturing the child’s full spectrum of strengths and needs.
That heterogeneity is why the treatment of each child focuses on the real impairment they are experiencing. For many children, well-managed stimulant medication can be a game-changer. It reduces the “noise” of inattention or hyperactivity so kids can develop coping skills and improve self-regulation. It can boost their self-esteem and ability to function in the family. Virtually all authorities agree that medication should be part of a multimodal treatment plan, accompanied by support when and where kids are struggling, including behavioral interventions. Sometimes, the child’s environment, such as a high-demand setting, will heighten ADHD symptoms and can be modified. Adjustments such as smaller class size or more physical activity can have a big impact.
A complex condition, not just school troubles
ADHD is a disorder that can impact far more than a child’s report card. Families often seek help not solely for problems in the classroom, but also because their child struggles at home, with hyperactivity and difficulty following rules, managing emotions, and handling social situations. And ADHD is not only a disorder of childhood. Research shows that untreated ADHD in adults elevates risks of car crashes, substance misuse, accidental injuries, and workplace challenges later in life. At all ages, ADHD symptoms vary by setting, but they can create significant distress and real consequences that require meaningful support.
What does neuroscience tell us?
Large-scale research consistently confirms that, on average, the brains of individuals with ADHD are subtly different in structure and function compared to those without the disorder. These differences often involve brain circuits crucial for attention, executive function, and impulse control. Like brain imaging findings for most other mental health conditions, the effect sizes are modest, and there’s significant overlap between individuals with and without ADHD. The takeaway? We still lack any single biological marker, or “brain scan test,” that can reliably diagnose ADHD in an individual child or adult. While ADHD involves genuine neurobiological factors, its complexity and heterogeneity mean there isn’t a simple, one-size-fits-all biological test. We’re making leaps in understanding ADHD at a group level, but we need more refined tools to pinpoint treatment paths for each child.
Why is the number of children with ADHD diagnoses on the rise?
Recent decades have seen incremental increases in ADHD diagnoses. Data from the CDC’s 2022 National Survey of Children’s Health indicated about 1 in 9 US children (11.4%) had ever received an ADHD diagnosis, roughly a million more than in 2016. Some of this increase is likely due to better awareness and more comprehensive screening. But environmental changes — like shifting school demands or pandemic disruptions — can also bring ADHD symptoms to the forefront in children who might otherwise have flown under the radar. Even kids with mild ADHD may feel overwhelmed if their environment is too demanding. A supportive setting can buffer them, while a stressful one can worsen symptoms.
Being alert to overdiagnosis can prevent labeling every restless child as having ADHD. But caution shouldn’t overshadow those who genuinely need help. The key is thorough evaluation to confirm persistent, clinically significant impairment, rather than transient restlessness or stress. Families also deserve an honest picture of our current science: While data-driven, personalized care is promising, it’s still years from daily clinical practice.
Medication effectiveness
The Times piece cites the results of the decades-old landmark Multimodal Treatment Study of ADHD (MTA), which demonstrated the effectiveness of stimulant medication for ADHD, as well as follow-up analyses that seemed to show no benefits after the three years of clinical treatment through the study.
But what that result showed was not that stimulants abruptly stop working after three years. It showed that medication effectiveness hinges on careful, systematic management — including correct dosing and regular monitoring — alongside therapies that address behavior and environment. In follow-ups after the study, insufficient dosing and a lack of follow-through, often seen in less structured community care, can explain many disappointing outcomes. The study also supported the value of combining medication with behavioral therapy for optimal outcomes, especially for improving behavior, parent-child interactions, and social skills.
Moving forward
The Times article closes with a recommendation that we conceive of ADHD as a mismatch between a child and his environment, and a prediction that in different environments, over a lifetime, people with ADHD may not always need stimulant meds to do well. This is certainly true — it’s an aspect of our increasingly nuanced understanding of the disorder, and the heterogeneity in the ways it presents.
That’s why it’s important to see stimulant medication as one tool — not the only tool — we have to help people with ADHD thrive. All children respond differently to changes in environment, and in the course of growing up many people with ADHD succeed in finding environments and roles in life that play to their strengths and minimize their struggles. At the Child Mind Institute, it’s our job to set them up with as many strengths and coping skills, and as much confidence, as we can to enable them to grow into their full potential.
The post Beyond the ADHD Headlines: A Nuanced Look at Diagnosis, Drugs, and Daily Life appeared first on Child Mind Institute.
]]>The post When Problem Behavior Masks a Learning Disability appeared first on Child Mind Institute.
]]>What was initially assumed to be anxiety or a behavior disorder turned out to be a learning disability. “When we assessed her, we found that she had dyslexia,” says neuropsychologist Angela Dewey, PhD. “She wasn’t being defiant — she was overwhelmed by reading and writing tasks.”
Children who struggle in school sometimes act out — resisting homework, refusing to participate, even becoming disruptive in class. To parents and teachers, it may come across as defiance or disinterest. But in many cases, these behaviors are signs of an undiagnosed learning disorder that can make school more challenging.
“A lot of times, parents come in saying their child is out of control,” says Dr. Dewey, who evaluates kids at the Child Mind Institute’s Gund Learning and Diagnostic Center. “What we sometimes find is that there’s an underlying learning issue that’s driving the behavior.”
Understanding the connection between behavior and learning disorders can help parents and educators provide the right support — and prevent children from falling behind academically and socially.
What is a learning disorder?
Learning disorders are rooted in how a child’s brain processes information. These neurological differences can make reading, writing, math, or paying attention much harder than for other kids. These difficulties are not due to a lack of intelligence or effort; rather, they stem from differences in brain function that make learning tasks more challenging.
Parents and teachers sometimes assume that a struggling child just isn’t trying hard enough. But as Dr. Dewey explains, “Kids do well when they can. If a child is acting out or refusing to do schoolwork, it’s usually not because they don’t want to learn. It’s because something is getting in their way.”
How learning disorders can look like behavior problems
When kids can’t explain their struggles, their frustration often shows up in their behavior or even physical symptoms. A child may become easily frustrated with homework, seem disorganized, or refuse to follow directions. Anticipating a difficult school day can make kids anxious, leading to meltdowns, avoidance, or physical symptoms such as stomachaches.
“A lot of times, we see children who have learning disorders come in with symptoms that are very consistent with anxiety,” Dr. Dewey says. “For example, some kids with undiagnosed learning disorders have significant school avoidance, shutting down or even refusing to go inside the building. Others may have meltdowns before school but manage to regulate their emotions once inside the classroom. If a child consistently struggles in a particular subject and reacts strongly to school-related stress, it could be a sign of an underlying learning disorder.”
Dyslexia: When reading leads to frustration
Dyslexia, a reading disorder, is one of the most common types of learning disabilities and often presents as a behavioral issue. A child who struggles to read may avoid reading assignments, refuse to read aloud, or become frustrated when asked to complete literacy-based tasks.
Children with dyslexia may also develop strategies to hide their difficulties. “Some kids become the class clown to distract from their reading struggles,” says Rachel Ganz, PhD, a neuropsychologist in the Gund Learning and Diagnostic Center at the Child Mind Institute. “Others may act like they don’t care or claim that reading is boring when, in reality, they’re struggling.”
Math and writing disorders: Avoidance and anxiety
Among the different types of learning disabilities, dyscalculia specifically impacts a child’s ability to work with numbers while dysgraphia affects their ability to write. Children with these disorders might procrastinate, “forget” assignments, or get upset when asked to do work specific to these areas.
Students with dysgraphia may struggle with handwriting, spelling, and organizing their thoughts on paper. “For some kids, writing a single sentence is exhausting and frustrating,” Dr. Ganz explains. “That frustration can lead to avoidance, and teachers might assume the child is just unmotivated.”
Dr. Ganz points out that school avoidance is often linked to learning difficulties. “Kids with undiagnosed learning disorders may feel sick before school, ask to go to the nurse, or frequently request bathroom breaks during class — especially before a difficult subject like reading or math.”
ADHD: Impulsivity mistaken for defiance
Although not technically a learning disorder, ADHD (attention-deficit hyperactivity disorder) also makes learning much more difficult. It is a neurodevelopmental disorder that affects a child’s ability to focus, regulate impulses, and manage tasks. Kids with ADHD may have trouble following directions, staying on task, or sitting still — behaviors that can be mistaken for defiance.
“Parents will say their child can focus for hours on video games but not on homework, so they must just be lazy,” Dr. Dewey says. “But that’s not the case. Kids with ADHD struggle to regulate their attention, which means focusing on non-preferred tasks is much harder for them.”
Additionally, ADHD can affect emotional regulation. “Kids with ADHD often have a low frustration tolerance,” Dr. Ganz says. “They might go from zero to one hundred in an instant — throwing a tantrum over a simple homework assignment because they feel overwhelmed.”
How learning disorders affect emotional well-being
It’s not only academics that suffer when a child has a learning disorder. They often affect a child’s social and emotional well-being, too.
“When kids struggle with academics, it often affects their confidence and self-esteem,” Dr. Dewey says. “They may feel embarrassed in front of their peers or worry about being called on in class. That anxiety can sometimes show up as avoidance, aggression, or complete shutdown.”
In some cases, children may develop anxiety or depression as a result of their struggles. “We see kids who internalize their academic difficulties, blaming themselves for not being smart enough,” Dr. Ganz says. “This can lead to feelings of worthlessness or even school refusal.”
Additionally, children with undiagnosed learning disorders may struggle with social interactions. They might have trouble keeping up with conversations, following rules in games, or remembering instructions. This can make it difficult to form friendships, leading to feelings of isolation.
Steps to take if you suspect a learning disorder
Recognizing the signs of different types of learning disabilities is the first step, but figuring out what to do next can feel overwhelming. Fortunately, there are clear steps parents and teachers can take to better understand a child’s struggles and put the right support in place.
Observe patterns
If your child’s behavior is raising red flags, the first step is to look for patterns. Are they struggling in a particular subject? Do they act out at certain times of the day? Identifying when and where the challenges occur can help uncover an underlying learning disorder.
Teachers and parents should track when behavioral issues occur. “If a child only acts out during reading or math, that’s a red flag that an underlying issue may be at play,” says Dr. Ganz. “Patterns give us important clues.”
Seek a professional evaluation
Many schools have the ability to evaluate students for learning disorders. Private neuropsychological testing is also an option in the event testing isn’t available at your child’s school, you disagree with the school’s findings, or you wish to gain more personalized insight into your child’s specific disability.
“Early intervention can prevent years of frustration,” Dr. Dewey says. “Without a diagnosis, kids may internalize their struggles and believe they’re just not smart enough — which isn’t true.”
Explore intervention strategies
Once a learning disorder is identified, the right support can make all the difference. With targeted interventions, children can develop the skills they need to succeed academically and feel more confident in their abilities.
- For dyslexia: Multisensory reading programs such as Orton-Gillingham or Wilson Reading System can help children strengthen their literacy skills. Parents and teachers can also encourage the use of audiobooks, provide extra time on assignments, and use phonics-based instruction to build reading confidence.
- For math and writing disorders: Structured, step-by-step teaching methods, graphic organizers, and hands-on learning strategies can make complex math concepts easier to grasp. Speech-to-text tools and extra time on assignments can also support children who struggle with writing.
- For ADHD: Executive function coaching, structured routines, and behavioral therapy can help children manage focus, organization, and self-regulation, making school tasks more manageable. Medication can improve students’ ability to focus.
Schools can also provide accommodations such as extra time on tests or modified assignments to support children with learning disorders.
Why early intervention matters
Early diagnosis and intervention can help children build confidence and avoid unnecessary frustration. “The earlier we identify a learning disorder, the sooner we can put supports in place,” Dr. Ganz says. “Getting a diagnosis isn’t about labeling kids — it’s about giving them the right tools to succeed.”
Frequently Asked Questions
Yes — behavior problems like meltdowns, school refusal, or defiance can be signs of an underlying learning disorder. When kids struggle with reading, writing, or math, they often feel overwhelmed or anxious, which can lead to acting out. Identifying a learning disability early can help address both the academic and behavioral challenges.
Common types of learning disabilities include dyslexia (difficulty with reading), dyscalculia (difficulty with math), and dysgraphia (difficulty with writing). Other related challenges, like auditory processing issues, can also impact learning. Each condition affects how a child processes information and may lead to frustration or avoidance in school.
The post When Problem Behavior Masks a Learning Disability appeared first on Child Mind Institute.
]]>The post Nurturing Communication in Kids With Autism appeared first on Child Mind Institute.
]]>Autism and early communication skills
In typically developing children, early social communication skills appear in a natural sequence, beginning with basic nonverbal communication — like looking at someone, pointing to something, or imitating what another person is doing. One of the earliest signs of autism is a delay in these early skills.
“In the same way that a child can’t run without first learning to sit up, stand, and take their first steps, there’s a predictable sequence that has to happen before social communication skills like language can develop,” explains Cynthia Martin, PsyD, the senior director of the Autism Center at the Child Mind Institute. She calls these early social building blocks “precursors to talk.”
These skills are the foundation not only for language but for many kinds of engagement and interaction as children grow, from playing with other kids to reading nonverbal cues to learning from other people.
The most effective early support for these skills in autistic children follows that same developmental sequence that occurs without prompting in neurotypical children. Helping them build these foundational skills has been shown to improve their ability to develop language and interact socially as they grow.
How to help kids build skills
The kind of therapy most experts recommend for helping kids develop communication skills is called naturalistic developmental behavioral intervention (NDBI). Naturalistic means that the teaching of skills occurs in a natural way — within the context of play or during a daily routine. Developmental means that it aims to help a child move though the typical sequence of development. Behavioral means that it uses strategies of behavioral therapy like reinforcing, modeling, and prompting. An intervention is a structured way to teach skills.
NDBIs aim to help kids develop social and communication skills in a play-based, child-led way. Parents can use NDBI techniques to enhance communication with their children at home, as part of everyday play and routines like getting dressed or brushing teeth.
Why are skills best developed in a ‘naturalistic’ way?
Earlier forms of training for young children with autism were more regimented. ABA, or applied behavior analysis, initially involved taking children through a predetermined set of exercises. But it was found that skills developed in the context of daily life are more likely to be remembered and used.
“It’s one thing to have a kid sit at a table in front of a set of three pictures, and say, ‘Find the T-shirt,’” Dr. Martin explains. “It’s a totally different thing to be at home and say, ‘OK, it’s time to get dressed. Find your T-shirt!’”
One popular NDBI program called Project ImPACT — which stands for Improving Parents as Communication Teachers — works with parents of children ages 1-8 who have social communication delays, including those who have been diagnosed with autism spectrum disorder. Since neurotypical children develop these skills without prompting, Dr. Martin notes, it’s not intuitive for parents to know how to nurture them.
What skills do very young children need to develop?
Project ImPACT identifies four groups of skills young children need to develop as building blocks for later, more sophisticated social interaction:
Social engagement: Using eye contact, facial expressions, gestures, and words to engage with others and share interests and attention. Social engagement is the basis of being able to learn from others.
Communication: Understanding and using facial expressions, gestures, sounds, words and sentences to interact. Children start with nonverbal communication, through eye contact and vocalization, then add gestures, like reaching, giving, and pointing, before they start using words. When children can’t communicate effectively they may develop problem behavior to try to get their needs met.
Imitation: Copying others helps children learn new skills and show interest in others. “Imitation is an important skill for kids to learn in the context of interactions with other people — it’s a way to connect with other kids — but also in the context of general learning,” adds Emilie Weiner, BCBA, a behavior analyst in the Autism Center at the Child Mind Institute.
Play: Interacting with toys and other objects for fun helps children learn social, motor, and problem-solving skills. Pretend play with other kids also strengthens the foundations for language skills.
Techniques for nurturing social communication skills
Project ImPACT teaches parents to use a set of techniques that have been shown in research to be effective for developing communication skills. These techniques include:
Focus on your child: Parents learn to start by joining their child in an activity of the child’s choosing, letting them lead the activity. Get face-to-face with your child and hold objects they are interested in near your face, to encourage them to look at you. Become part of the play by handing them things or imitating what they are doing. If they are playing with cars, get another car and imitate what they’re doing. If they are splashing in the bath, splash with them.
Use animation: Show excitement about your child’s activity, using big gestures and exaggerated facial expressions. Use simple language to talk about what you and the child are doing. Vary the volume and pitch of your voice, to make it stand out to your child. Use attention-getting words and phrases like “Wow!” and “Oh no!” Then wait and watch for their attention. When you get a reaction, respond with simple language and imitate what they are doing.
Model and expand communication: Use simple language to talk about what you and your child are doing. Stress important words and repeat them several times. Expand your child’s communication by adding new words. The idea, explains Dr. Martin, is that you match your language to whatever length your child’s utterances are and then go up one more word. “So if your child is predominantly speaking in one to two words, then you need to limit what you’re saying to two to three words. And you want to phrase things as statements, not questions.”
Create opportunities: Prompt your child to show or tell you that they want something by setting up an opening and then waiting and watching. The key is that you don’t just anticipate what their needs are, says Alexis Bancroft, PhD, a psychologist in the Autism Center at the Child Mind Institute. “Maybe you say something like ‘What do you want?’ Then you wait for them to look at you or show you in whatever way they can and then give them the thing they want.”
Playfully obstruct: One way to prompt communication is to playfully block a child’s activity and wait for them to respond. You start by choosing a word or phrase to warn them you are about to interrupt. If they’re pushing a car, you can say, “Beep, beep!” and block the car with another car. Wait for a response, and then move the car and say, “Move!”
Take balanced turns: Introduce the idea of taking turns by watching your child, narrating what they are doing, and then taking a turn yourself. When you take a turn, you model play skills. “If you are building with blocks, you model a new way they could build with blocks,” says Ms. Weiner. “You’re modeling behaviors and skills that you want your child to seize or to engage in, but not forcing them to engage in them.” Having two sets of toys can facilitate this kind of interaction. “With your set, first you imitate what your child is doing, and then you model a new way to do it and narrate what you are doing,” explains Dr. Martin.
Set up communicative temptations: Put fun things in sight but out of reach to prompt your child to say or show you what they want. Offer one cracker and prompt them to ask for more. “Instead of them just helping themselves to the snacks, you create a little barrier,” says Dr. Bancroft, “so that the child has to take that extra step.” Instead of having all the toys out and available, you might put things on a shelf where the child can see but not reach them without your help, or in bins where the child can see them, but they can’t open them themselves.
Teach new skills: At whatever level your child is communicating, prompt them to use a slightly more complex skill by modeling it, and reward new behavior.Pause before giving a prompt, gain your child’s attention, and use simple language. Use only one prompt at a time, then give the child time to respond, such as counting to five in your head before giving another prompt. If you need to prompt a third time, give more support so they can be successful, such as helping them point to it. For instance, if you want the child to point to bubble toy, the first prompt might be to show your child the toy and wait. The second might be to say, “What do you want?” The third might be to help them point to the bubble toy.
Building a reciprocal relationship
Project ImPACT recommends using these techniques during as many activities as possible, and outside the house as well as at home. And while the goal of using them is to encourage children to engage and communicate more, there are benefits for parents, too.
These techniques can also help parents connect with kids who don’t respond typically. “When an autistic child doesn’t respond as much as a parent might hope — like not making eye contact, smiling back, or showing interest — the parent may start to feel discouraged,” explains Dr. Bancroft. “Because they’re not getting that response, a parent might naturally pull back a bit themselves. But when parents have tools to help their child engage more, it can really strengthen that back-and-forth connection. It supports a more mutual, rewarding relationship between parent and child.”
Frequently Asked Questions
One of the earliest signs of autism is a delay in nonverbal social behaviors, like looking at others, pointing to show interest, or copying actions. These behaviors, which develop without prompting in neurotypical children, are essential building blocks for language.
Naturalistic Developmental Behavioral Interventions (NDBIs) are often recommended because they mirror how children naturally learn — through play and daily routines. NDBIs are play-based, follow the child’s lead, and use strategies like modeling, prompting, and reinforcing skills to build. These approaches help children learn in meaningful ways and are more likely to result in lasting communication improvements.
Parents can support their child’s language development by:
- Following the child’s lead during play
- Using exaggerated facial expressions and animated speech
- Repeating and expanding on the child’s vocalizations
- Creating communication opportunities by pausing and waiting for a response
The post Nurturing Communication in Kids With Autism appeared first on Child Mind Institute.
]]>The post The Child Mind Institute Secures $4.25 Million Grant From the Morgan Stanley Foundation to Transform School Mental Health appeared first on Child Mind Institute.
]]>The training will equip educators and school-based clinicians with tools to teach preventative mental health skills, including emotional awareness, coping strategies, conflict resolution, and mindfulness. The expansion will initially focus on New York and California, where the Child Mind Institute has operated programs in more than 320 schools, before rolling out to other states. This initiative is a critical step toward addressing the growing demand for accessible mental health resources in educational settings.
“Our partnership with the Morgan Stanley Foundation marks a transformative moment in the effort to ensure every child has access to quality mental health support,” said Dr. Harold S. Koplewicz, founding president and medical director of the Child Mind Institute. “By equipping educators and school mental health professionals with the tools they need to support students, we’re creating sustainable change that will benefit students and school communities across the country for years to come.”
The work of this grant builds on the successful partnership between the Child Mind Institute and Morgan Stanley. In 2020, the Child Mind Institute joined the Morgan Stanley Alliance for Children’s Mental Health (“the Alliance”), which brings together leading nonprofits and supports transformative initiatives that strategically address the growing crisis in children’s mental health.
The Alliance has been instrumental in ensuring the accessibility of the Child Mind Institute’s Family Resource Center, a hub of over 1,000 articles and guides on children’s mental health and learning disorders rooted in the latest research and informed by expert clinicians. Over 47 million unique visitors have accessed the Family Resource Center since its 2021 relaunch. The Alliance has also supported Child Mind Institute studies on COVID-19’s effects on the mental health of children and families, problematic internet usage, as well as upcoming work related to intergenerational stressors and support for families.
“The Alliance has made much-needed strides to foster awareness, collaboration and innovation to ensure that children have the mental health support they need to grow and thrive,” said Joan Steinberg, President of the Morgan Stanley Foundation and CEO of the Alliance Advisory Board. “We are grateful for the Child Mind Institute’s ongoing partnership and their important contributions in addressing today’s youth mental health crisis.”
For more information about this program and the Child Mind Institute, please visit https://childmind.org/school-and-community/.
To learn more about the Alliance, please visit https://morganstanley.com/mentalhealthalliance.
About the Child Mind Institute
We are the leading independent nonprofit in children’s mental health providing gold-standard, evidence-based care, delivering educational resources to millions of families each year, training educators in underserved communities, and developing open science initiatives and tomorrow’s breakthrough treatments.
Visit Child Mind Institute on social media: Instagram, Facebook, Twitter, LinkedIn
For press questions, contact our press team at childmindinstitute@ssmandl.com or our media officer at mediaoffice@childmind.org.
The post The Child Mind Institute Secures $4.25 Million Grant From the Morgan Stanley Foundation to Transform School Mental Health appeared first on Child Mind Institute.
]]>The post Why ‘Adolescence’ has everyone talking about raising good men appeared first on Child Mind Institute.
]]>The post Why ‘Adolescence’ has everyone talking about raising good men appeared first on Child Mind Institute.
]]>
Social challenges